Effects of Occupational Radiation Exposure on the Physician Workforce: Current Scope, Implication, and the Path Forward
Executive Summary
The use of intraoperative imaging has drastically improved surgical safety and outcomes and has become the standard of care across a wide range of procedures. However, its use is associated with cumulative scatter radiation exposure, placing surgeons and operating room staff at elevated risk of malignancy and other harmful health-related effects. Over the years, many different measures have been put into practice to mitigate the harmful effects of this radiation exposure. Additionally, new innovations in imaging technologies have allowed for reduced radiation exposure. Despite these developments, surgeons remain at high risk for adverse outcomes from this occupational hazard. Here, we discuss the background of this issue, the pathophysiology of these harmful effects, current mitigation strategies and policies, and the path forward to providing a safer working environment.
Introduction
The use of ionizing radiation for medical imaging is essential to both diagnosis and treatment in modern healthcare, yet it poses an occupational risk to practitioners.1 While a patient may undergo a few scans over the span of years, physicians are potentially exposed to radiation daily as they use imagining techniques to aid in their performance of procedures.1 The cumulative effects of this radiation exposure throughout one's career are still largely unknown, but several studies identify that certain physicians regularly using intraoperative imaging are at increased risk of several cancers.1 As the use of fluoroscopy and intraoperative CT is growing and more specialists are performing these procedures, it is crucial to address the threat they pose to physicians.1 Understanding this risk is essential to mitigating it through prevention and screening targeted towards this population. We will define ionizing radiation as an occupational risk for physicians, describe the status of current research demonstrating harmful health effects, explore current risk management, and address the need for further mitigation efforts.
Ionizing Radiation Uses in Healthcare
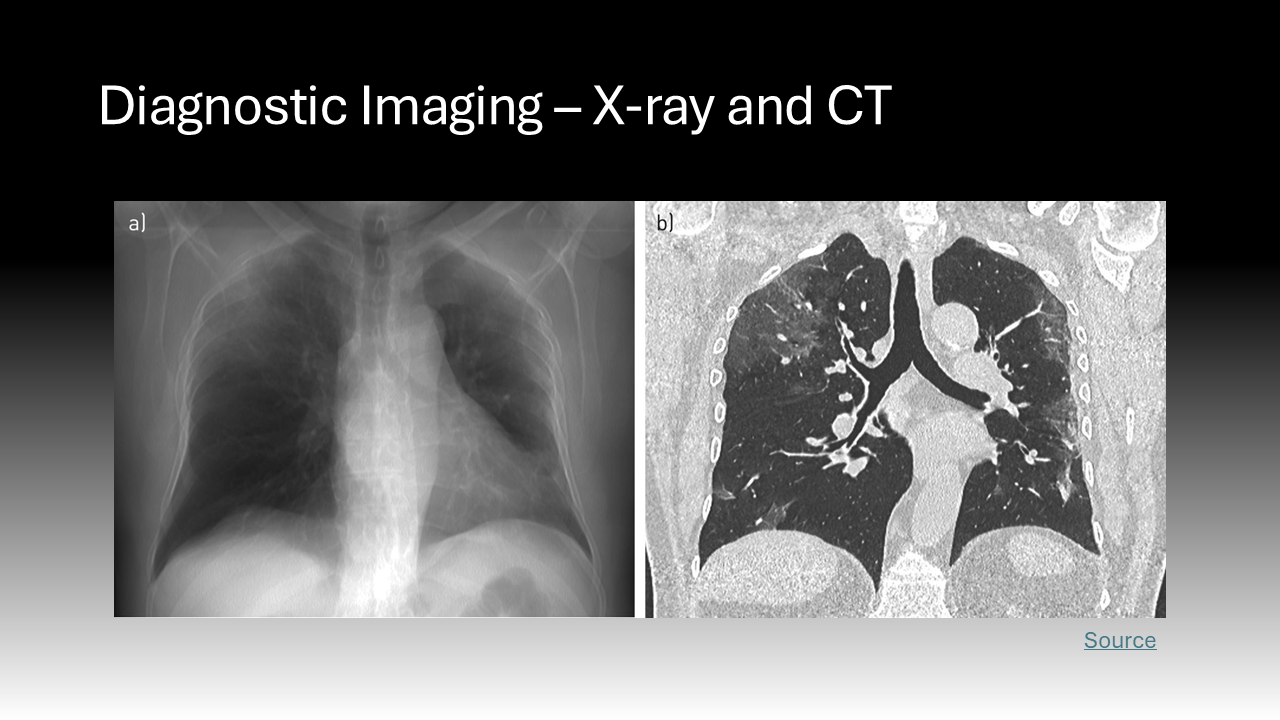
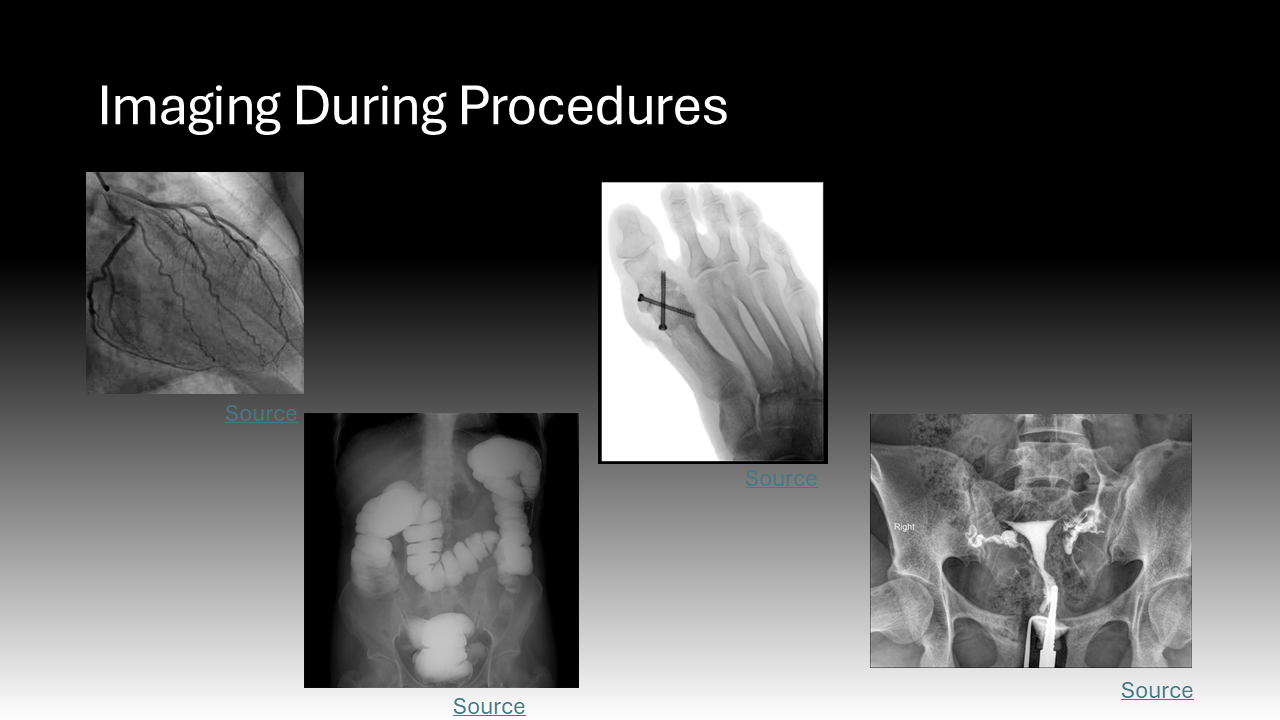
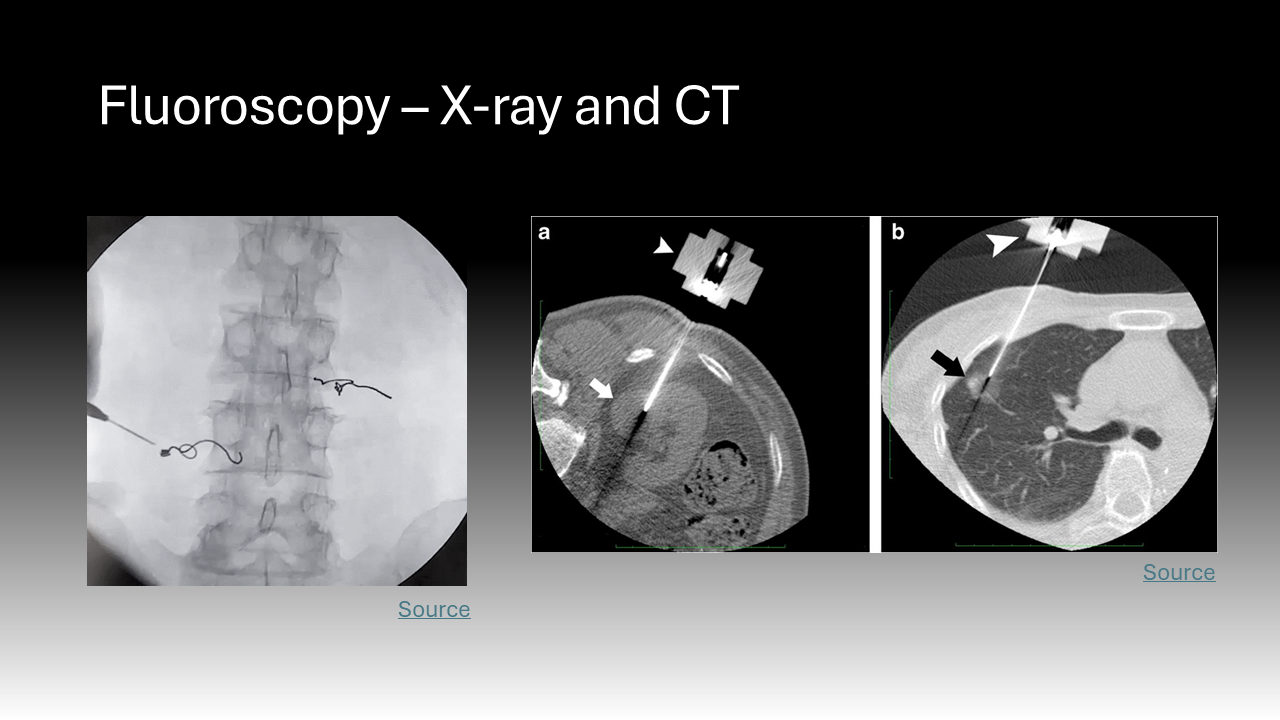
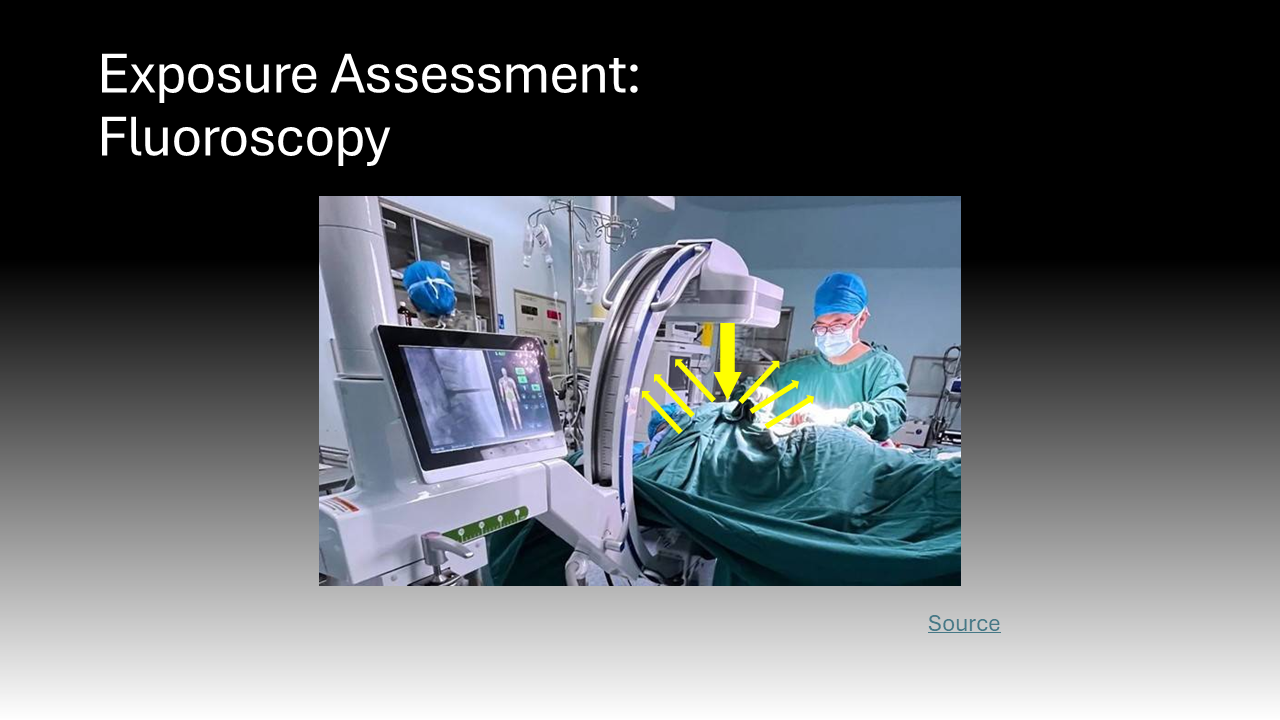
Ionizing radiation encompasses all high-energy rays that detach electrons from atoms. The body absorbs a fraction of this energy, which is disruptive at the molecular level.2 Ionizing radiation is found at low levels in the natural environment but has been employed at higher doses in medicine since the late 19th century.3 X-rays are ubiquitous in healthcare; this ionizing radiation has been the basis of two-dimensional diagnostic images and CT scans for years but is now employed during procedures.3 Cardiologists, neurosurgeons, orthopedic and vascular surgeons, and interventional radiologists all use live, continuous fluoroscopic imaging intraoperatively for “real-time feedback” during procedures.4 This technology not only allows for more accurate interventions but enables the use of minimally invasive approaches that replace open surgeries.4 In sum, the expanding use of X-ray technology in medicine, especially over the past 20 years, has led to more efficient diagnosis and treatment that is safer and more tolerable for patients.5 However, it also exposes a more diverse number of physicians to radiation and its harmful effects.5 Whereas X-rays during a diagnostic image or cancer radiation treatment are delivered to a physically isolated patient, physicians must be in close proximity to patients and radiation sources to perform procedures.5 This creates the current dilemma where healthcare providers now comprise the largest group of workers exposed to radiation in the world.5
Doses of Radiation Experienced by Physicians
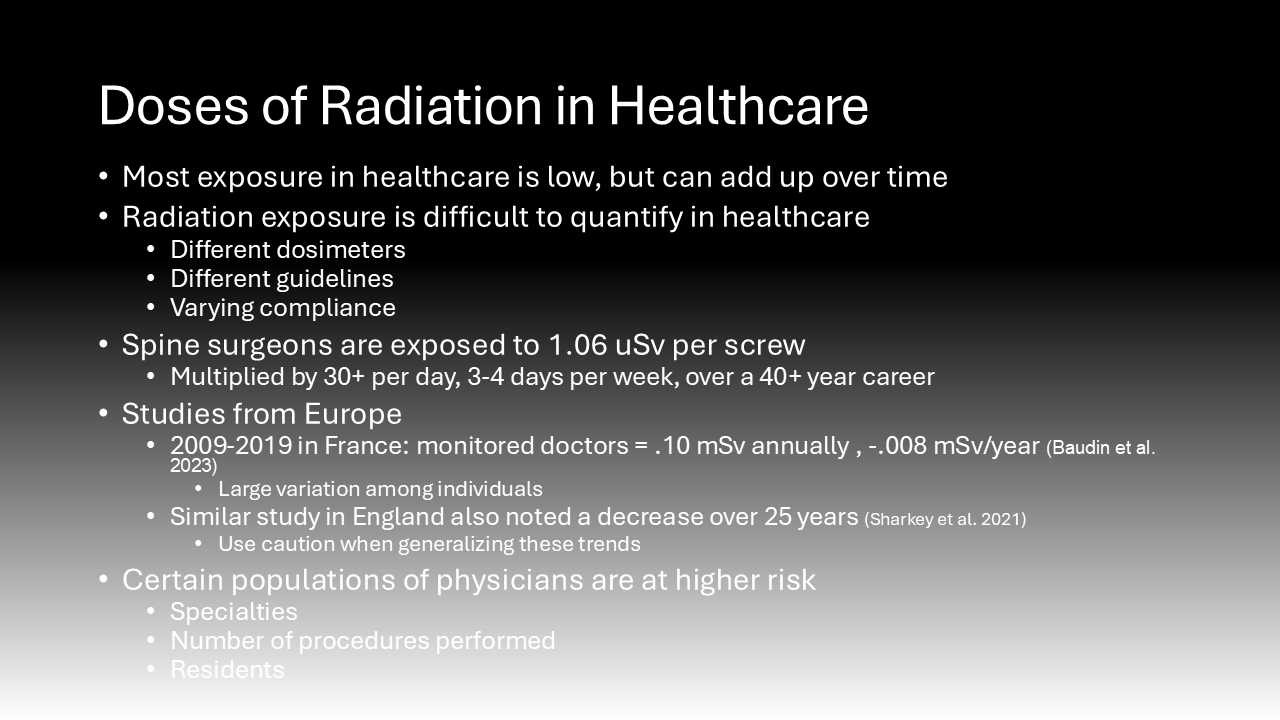
The effects of radiation are dose-dependent.6 This means that while the potential damage from the low doses of radiation used during a medical procedure is slight, it is the cumulative effects of this chronic exposure in healthcare workers that are worrisome.6 It is logistically challenging to track radiation exposure in the healthcare setting because there are different types of dosimeters and various sets of guidelines for their use that differ by institution.7 Additionally, though they are mandated to wear dosimeters, individuals vary in their compliance with safety practices and protective shield use, which will be discussed later.7 While data on US physicians is lacking, several retrospective cohort studies in Europe have determined levels and trends of radiation exposure in healthcare workers.7 The standard unit for radiation is a gray (1 joule of energy absorbed by 1 kilogram) but when considering the harmful effects of radiation, grays are multiplied by a quality factor to convert to Sieverts (Sv).4
The use of fluoroscopy mainly exposes surgeons to scatter radiation, which is a lower dose as opposed to direct radiation that patients experience.8 However, this scatter radiation exposure in physicians accumulates significantly over time. Prior investigation demonstrates that spine surgeons using fluoroscopy are exposed to an average of 1.06 uSv per screw.8 Spine surgeons may place as many 30+ screws per day, 3-4 days per week, multiplied over a 40-year career.8 To put this in perspective, studies of survivors of the Hiroshima bombing have shown that being exposed to just one Sv is associated with a 60% increased chance of developing a solid malignancy.8 While the use of fluoroscopy is critical for patient safety and surgical success, the exposure experienced by physicians accumulates significantly over time.8
Few studies abroad have attempted to quantify trends in occupational exposure to radiation among physicians over time. One study of three hospitals in France determined that monitored healthcare workers were exposed to .10 mSv annually, averaged from 2009 to 2019, with a -.008 mSv/year trend. This translates to a 58% decrease over that 10-year period.5 However, there was considerable variation between individuals, with some experiencing 0 Sv while others experienced several tenths of a Sv each year.5 Another study conducted in England over 25 years determined that the radiation dose experienced by doctors in their cohort similarly decreased.9 While this data seems promising in that it demonstrated a reduced radiation dose experienced by physicians despite increased use of the technology, the authors of both studies warn of false reassurance.9 They state that these results may not be widely applicable due to increased monitoring and regulation of European working hours.9 Additionally, they attribute much of the decrease in exposure observed to an increase in the number of dosimeters reporting zero dose, which could be due to the dose falling below the detection limit of .05 mSv.5 This means that while lower doses of radiation may be used and are below the detection capabilities, we are unsure how their cumulative effect could add up.5 The authors warn that despite this measured trend, the risks of exposure to ionizing radiation in the healthcare field are still significant.9
It is important to note that these studies on the average dose of radiation experienced by physicians annually do not account for the heterogeneity that leads to some physicians being exposed to much higher doses than average.7 For instance, based on the duration of training and the number of procedures performed, one study concluded that neurosurgeons experience greater radiation doses than doctors in other specialty programs that use intraoperative imaging.7 Additionally, another study found that comparatively few anesthesiologists were issued dosemeters compared to surgeons when they, too, were exposed to radiation.9 The literature also likely underestimates the dose of radiation experienced by physicians in residency training for several reasons.9 Residents may wear lead protection less frequently due to the lax attitudes of some supervising staff who trained when radiation safety was less emphasized.7 These physicians-in-training are less likely to have properly fitting lead protection due to the costs associated with its purchase.10 Finally, residents often overuse intraoperative imaging compared to attending physicians performing the same procedure due to their inexperience and higher dependence on checking their work with images.7 The combination of these confounding factors necessitates caution when generalizing the results of studies demonstrating that radiation doses are down-trending.7 Additionally, although increased dose leads to increased risk, it is essential to remember that no level of radiation exposure is considered “safe.7”
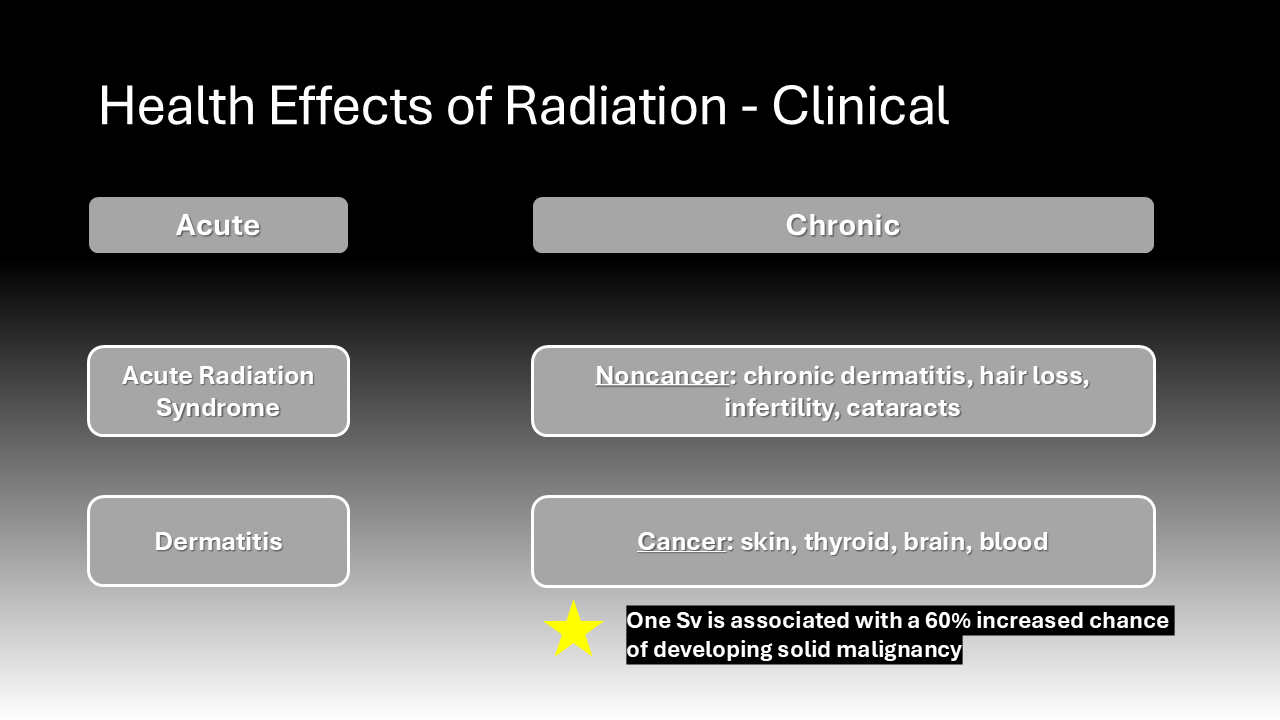
Health Effects of Radiation Exposure
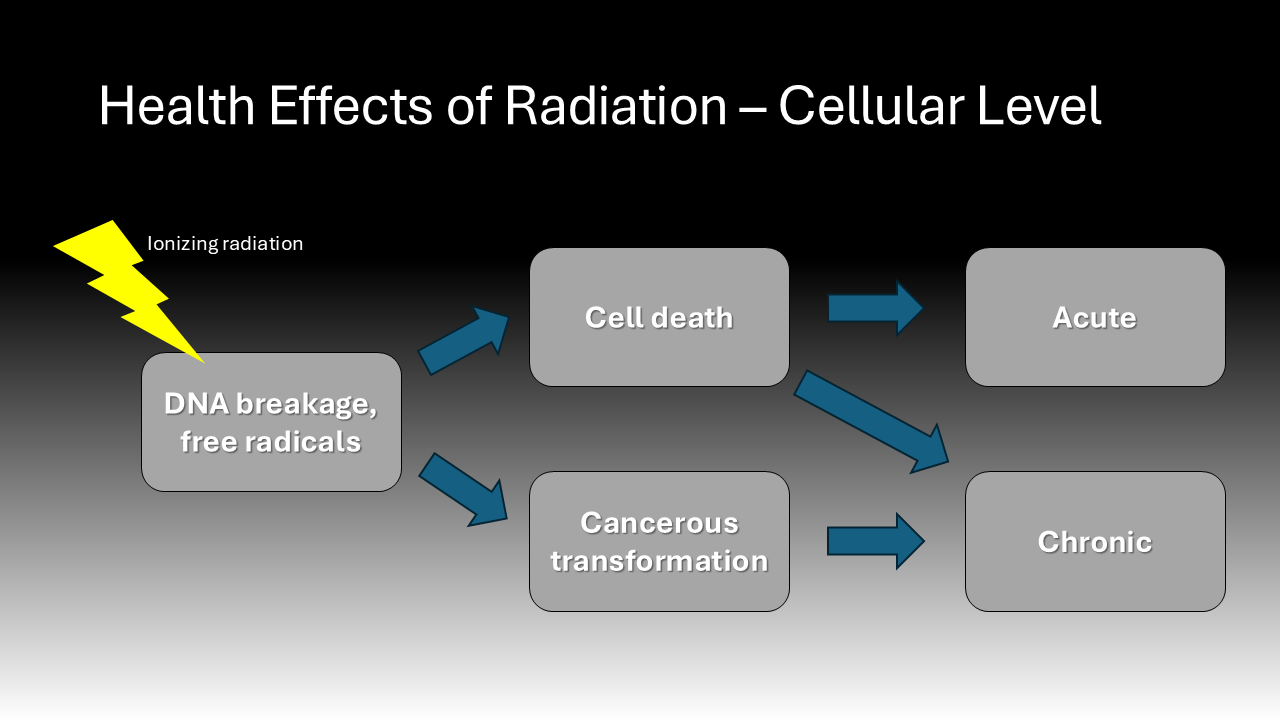
The health effects of radiation exposure have been known since the immediate years following the introduction of X-ray technology when there was noted to be an increase in incidence of cancers among workers.11 More recent molecular research elucidates the mechanism by which radiation leads to deleterious effects. Ionizing radiation causes DNA breakage and mutation directly and through the generation of free radicals.11 One study found that molecular markers of DNA damage and repair were increased among the lymphocytes of patients and hospital staff immediately post-operatively when fluoroscopy was used.12 This resulting genetic instability may either kill a cell or cause it to become cancerous.12 The clinical effects of radiation exposure depend on the dose and duration of exposure. High doses can lead to severe skin damage and acute radiation syndrome, almost all exposure in healthcare involves low doses over long periods.4 While chronic exposure to low doses of radiation can lead to non-cancer effects such as dermatitis, cataracts, and infertility, the focus of this paper is on the cancer effects.6 Most quantifications of cancer risk due to radiation derive from studies on the impact of atomic bombs. Data from Hiroshima and Nagasaki, Japan, demonstrated that radiation exposure increases the risk of a variety cancer types, specifically skin, thyroid, brain, and blood cancers.7 Data from survivors of the atomic bombs was extrapolated to estimate that an exposure of 10 mSv confers a 1 in 2,000 risk of developing cancer of any origin.7 Studies of radiologists in the 1950s further substantiated the link between radiation exposure and the previously mentioned cancer types.13
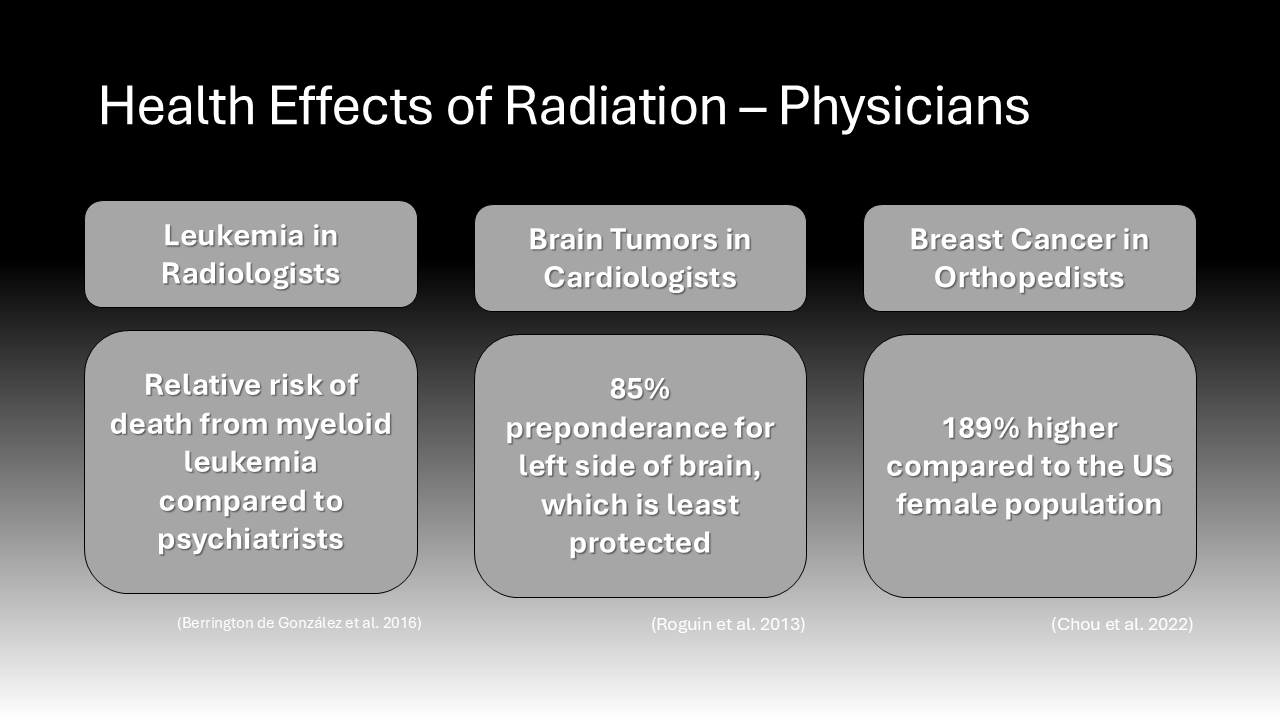
Observed trends of increased specific cancer incidence in physicians of certain specialties renew the community’s concern over the effects of radiation exposure. Clusters of cancer types seem to be correlated with occupational radiation exposure by physicians. For instance, a cohort study comparing 43,000 radiologists to a control group of psychiatrists found that the relative risk of death from myeloid leukemia was 1.43 in the radiologists.11 Another study found that a group of cardiac interventionalists with radiation-associated head and neck tumor subtypes, such as glioblastoma, had a disproportionate number of brain tumors originating on the left side of the brain. Eighty-five percent of the physician’s tumors were left-sided, while in the general population, brain tumors are equally likely to occur on either side of the brain.14 The researchers explained this preponderance of left-sided brain tumors by the fact that the left side of the head typically experiences the highest burden of radiation as it is least protected by the typical shields.14 This supports the conclusion that shared radiation exposure during procedures increases cancer risk in this group. Furthermore, numerous studies demonstrate a higher incidence of breast cancer among female orthopedic surgeons compared to the general population and other surgeons not exposed to radiation.10 A recent study contacting 1290 female orthopedic surgeons determined that the prevalence of breast cancer was 189% higher among this group compared to the US female population, even after adjusting for age and race.10 While the increased risk for breast cancer in this cohort might be attributable to delaying childbearing, this cohort had many more lifestyle factors that were protective against breast cancer, such as normal weight.10 This suggests that their occupational exposure to radiation in surgery was significant enough to increase their risk of breast cancer. In sum, there is a considerable amount of data suggesting that physicians exposed to radiation from the use of intraoperative imaging technology are at an increased risk of developing several types of cancer and new evidence continues to emerge.
Current Mitigation Strategies
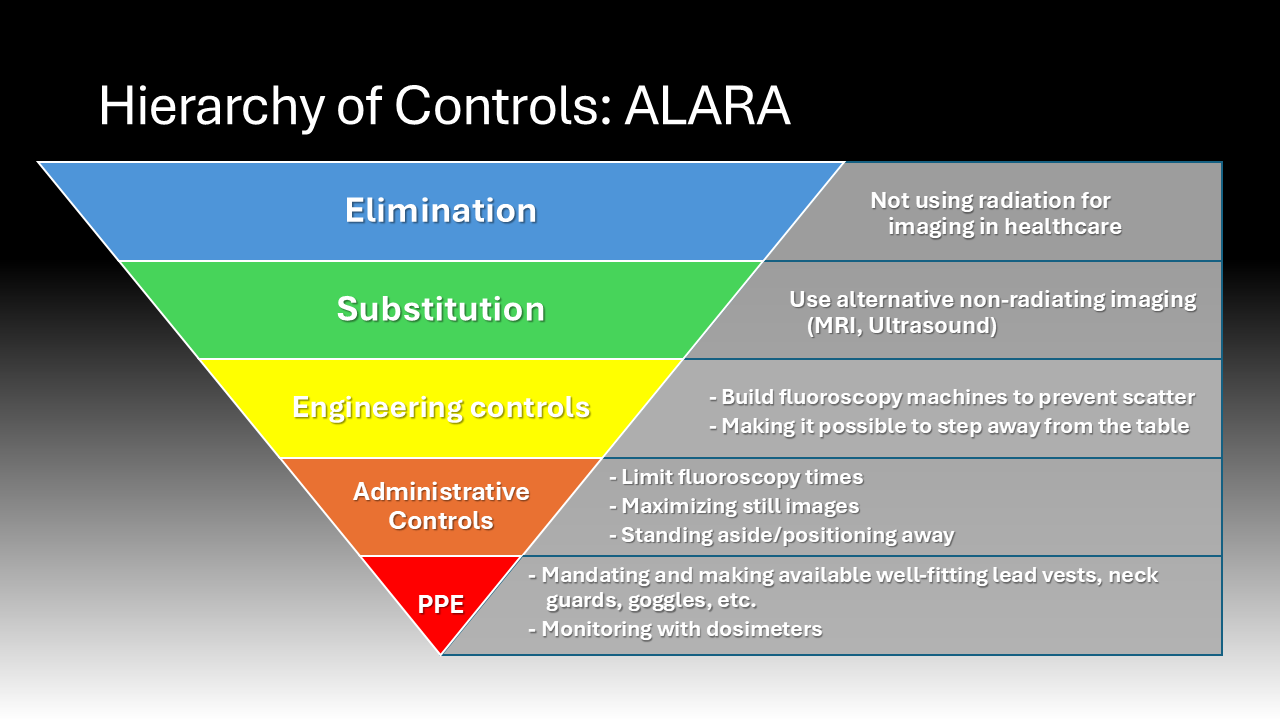
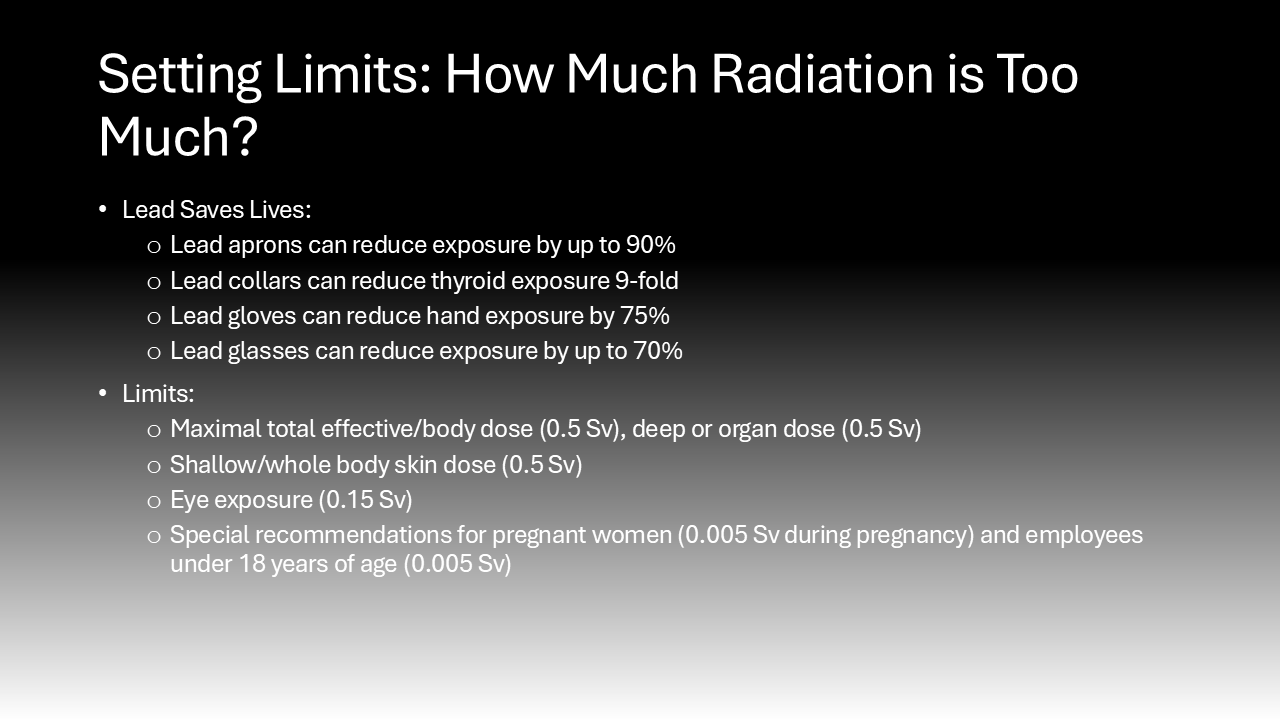
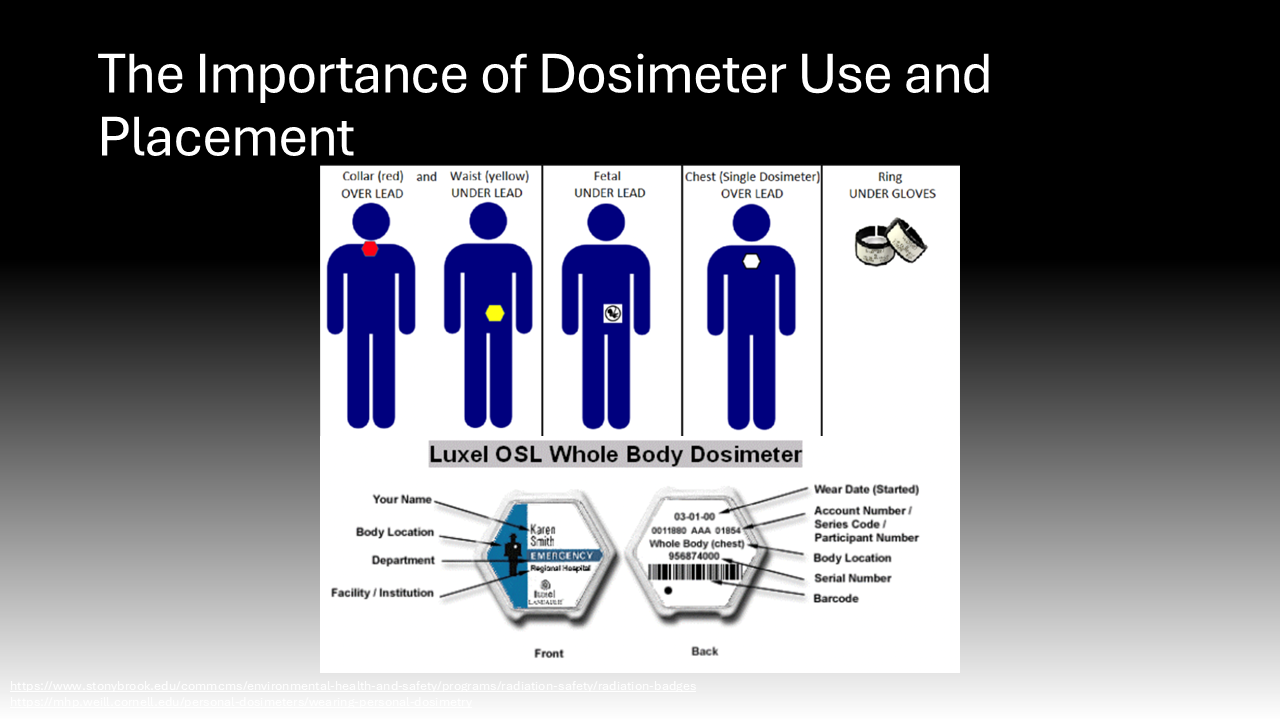
In the operating room, the core tenet of risk mitigation from intraoperative radiation exposure is known as “ALARA,” as low as reasonably achievable.6 This means surgeons are encouraged to use the lowest amount of radiation to achieve a safe surgical environment and outcome.6 To achieve ALARA, it is essential that surgeons wear dosimeters while in the OR to quantify their radiation exposure so it can be tracked by hospital occupational safety experts.15 Understanding their exposure is essential to alert them to their increased risk so they can accordingly mitigate radiation exposure. Many organizations and institutions set dose limits for radiation exposure for their physicians. For instance, the Cleaveland Clinic, a leader in the medical field sets the following annual limits of radiation exposure for their physicians: a maximal total effective/body dose (0.5 Sv), deep or organ dose (0.5 Sv), shallow/whole body skin dose (0.5 Sv), eye exposure (0.15 Sv), and special recommendations for pregnant women (0.005 Sv during pregnancy) and employees under 18 years of age (0.005 Sv).6
Several practices in the operative setting can reduce the quantity and severity of radiation exposure.6 These range from the most effective practices on the hierarchy of controls including elimination and substitution of ionizing rays for other imaging techniques to donning personal protective equipment. Ideally, new advancements in imaging technology would allow the substitution of ionizing radiation for safer imaging modalities which may include magnetic resonance imaging (MRI) or ultrasound. Additionally, there is also a lot of effort being allocated towards developing new intraoperative imaging modalities that use lower doses of X-ray without sacrificing the image quality and utility.6 Unfortunately, while ionizing radiation use intraoperatively could be substituted in future, it is currently still a mainstay in the operating room. Surgeons are encouraged to mitigate their risk of radiation exposure through the ways they use intraoperative imaging. For instance, using single images, slow frame and pulse rates, low magnification, and short fluoroscopy run times when feasible can reduce their exposure.6
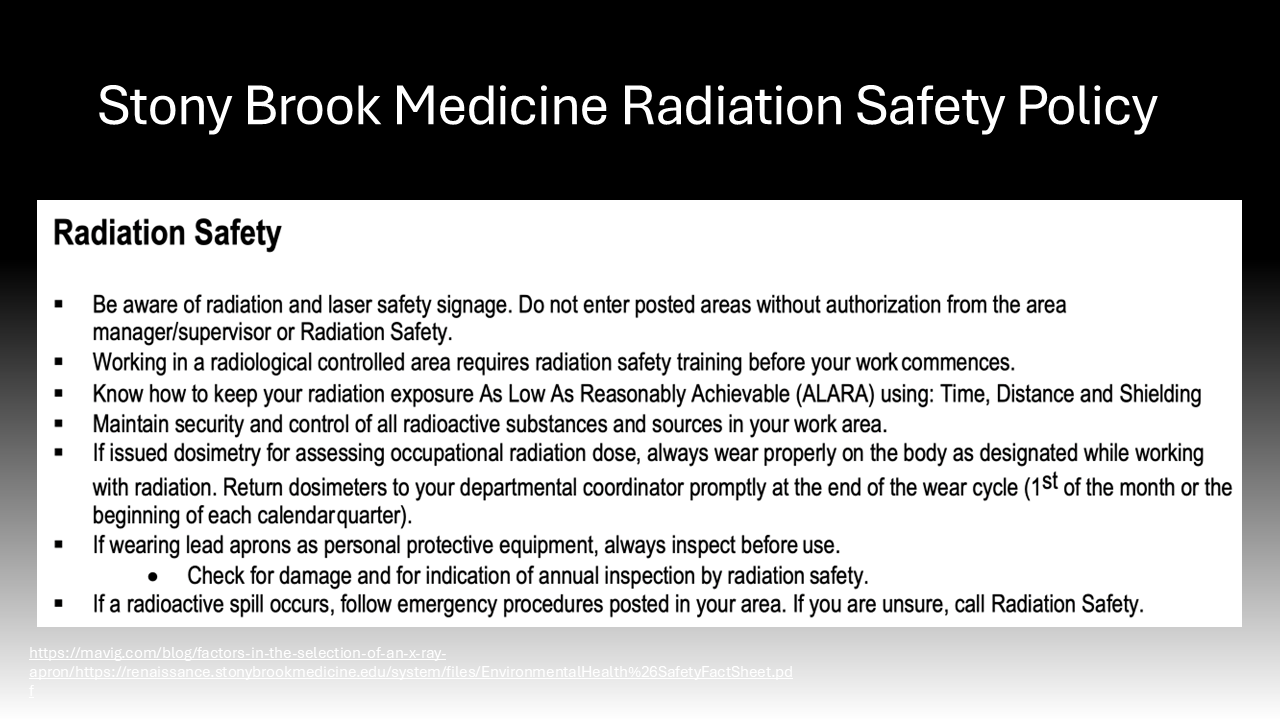
Behavioral modifications and personal protective equipment also play a key role in risk mitigation for those exposed to intraoperative radiation.4 When surgeons stand further away from the radiation source, they are exposed to an inversely proportionally decreased dose of radiation.4 Additionally, simply standing on the same side as the receiver significantly reduces the exposure to the scattering radiation as it bounces off the receiver.4 Following the establishment of the Advisory Committees on X-Ray and Radium Protection in the late 1920s, recommendations and regulations requiring the availability and use of lead protection devices and shielding devices have significantly curbed the negative effects of intraoperative scatter radiation exposure.16 These policies were adopted by the Occupational Health and Safety Administration (OSHA) and local hospitals, such as Stony Brook University Hospital.17–20 Lead aprons can reduce exposure by up to 90%, lead collars can reduce thyroid exposure 9-fold, lead gloves can reduce hand exposure by 75%, lead glasses can reduce exposure by up to 70%, and shields can offer significant reductions.4,21
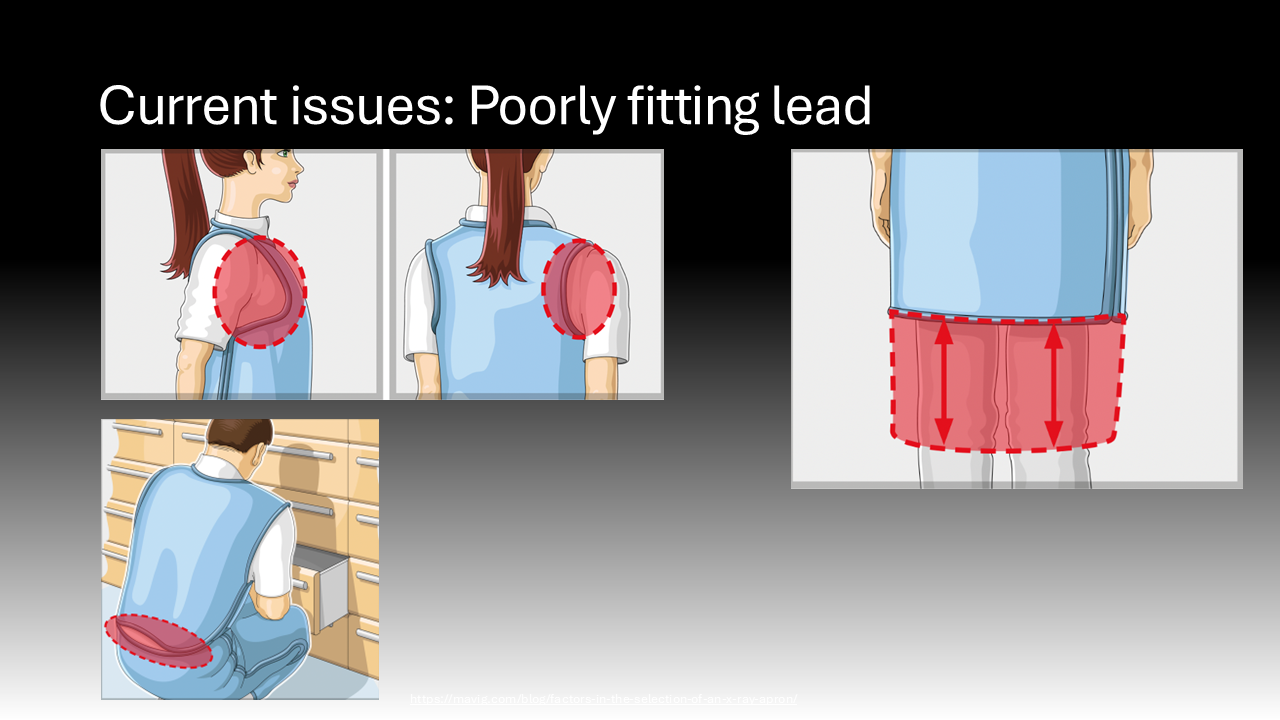
The major caveat to the efficacy of lead aprons is their fit. Many of the lead aprons historically have come in “unisex” sizing, tailored for men, leaving certain parts of women’s bodies poorly protected.4,13 This is particularly problematic in fully protecting the entirety of the breast tissue that is at high risk for malignancy.4,13 This may partly be mitigated for attending surgeons who are able to purchase their own lead or have their department purchase lead for them.4,13 However, trainees are often left scavenging for lead that fits poorly, placing them at unnecessarily high risk.10,13 It is critical to ensure that trainees have easy access to effective mitigation tools to ensure their health and wellness. Additionally, lead garments are heavy and cumbersome, which may discourage their use.
Future Mitigation: The Path Forward
One of the most significant deficiencies in this field is a knowledge gap – in a survey of 1,121 orthopedic surgeons, 75% of those polled reported they had no knowledge of the harmful effects of fluoroscopy despite knowing how it works and using it daily.15 The authors also found that only 63% of the surgeons were assisted by X-ray technicians who were familiar with the intricacies of their cases, resulting in an elevated average of 54.5 shots with fluoroscopy per case.15 And most alarmingly, just 5% of surgeons polled used dosimeters.15 The path forward must involve a variety of interventions. These should include heavy education efforts for surgeons and support staff, increasing the availability and mandating the use of protective equipment, ensuring regular monitoring of radiation exposures, investing in new and safer modes of effective intraoperative imaging, and fostering a collaborative culture of safety in the operating room environment.


References
1. Linet MS, Kim KP, Miller DL, Kleinerman RA, Simon SL, Berrington de Gonzalez A. Historical review of occupational exposures and cancer risks in medical radiation workers. Radiat Res. 2010;174(6):793-808. doi:10.1667/RR2014.1
2. Us Epa O. Radiation health effects. Published online November 12, 2014. Accessed June 22, 2024. https://www.epa.gov/radiation/radiation-health-effects
3. UpToDate. Accessed June 22, 2024. https://www.uptodate.com/contents/radiation-related-risks-of-imaging?search=ionizing
4. Wan RCW, Chau WW, Tso CY, et al. Occupational hazard of fluoroscopy: An invisible threat to orthopaedic surgeons. J Orthop Trauma Rehabil. 2021;28:221049172110355. doi:10.1177/22104917211035547
5. Baudin C, Vacquier B, Thin G, et al. Occupational exposure to ionizing radiation in medical staff: trends during the 2009–2019 period in a multicentric study. Eur Radiol. 2023;33(8):5675-5684. doi:10.1007/s00330-023-09541-z
6. Clinic C. Radiation a danger to patients and physicians alike. Cleveland Clinic. Published January 15, 2015. Accessed June 22, 2024. https://consultqd.clevelandclinic.org/radiation-a-danger-to-patients-and-physicians-alike
7. Zaidi HA, Montoure A, Nakaji P, Bice A, Tumialán LM. A 5-year retrospective analysis of exposure to ionizing radiation by neurosurgery residents in the modern era. World Neurosurg. 2016;86:220-225. doi:10.1016/j.wneu.2015.09.059
8. Jenkins NW, Parrish JM, Sheha ED, Singh K. Intraoperative risks of radiation exposure for the surgeon and patient. Ann Transl Med. 2021;9(1):84-84. doi:10.21037/atm-20-1052
9. Sharkey AR, Gambhir P, Saraskani S, et al. Occupational radiation exposure in doctors: an analysis of exposure rates over 25 years. Br J Radiol. 2021;94(1127). doi:10.1259/bjr.20210602
10. Chou LB, Johnson B, Shapiro LM, et al. Increased prevalence of breast and all-cause cancer in female orthopaedic surgeons. J Am Acad Orthop Surg Glob Res Rev. 2022;6(5). doi:10.5435/jaaosglobal-d-22-00031
11. Accessed June 22, 2024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5131832/#:~:text=The
12. El-Sayed T, Patel AS, Cho JS, et al. Radiation-induced DNA damage in operators performing endovascular aortic repair. Circulation. 2017;136(25):2406-2416. doi:10.1161/circulationaha.117.029550
13. Linet MS, Kim KP, Miller DL, Kleinerman RA, Simon SL, de Gonzalez AB. Historical review of occupational exposures and cancer risks in medical radiation workers. Radiat Res. 2010;174(6b):793-808. doi:10.1667/rr2014.1
14. Roguin A, Goldstein J, Bar O, Goldstein JA. Brain and neck tumors among physicians performing interventional procedures. Am J Cardiol. 2013;111(9):1368-1372. doi:10.1016/j.amjcard.2012.12.060
15. Tunçer N, Kuyucu E, Sayar Ş, Polat G, Erdil İ, Tuncay İ. Orthopedic surgeons’ knowledge regarding risk of radiation exposition: a survey analysis. SICOT J. 2017;3:29. doi:10.1051/sicotj/2017008
16. ICRP. Accessed June 22, 2024. https://www.icrp.org/
17. Accessed June 22, 2024. https://renaissance.stonybrookmedicine.edu/system/files/EnvironmentalHealth&SafetyFactSheet.pdf
18. Accessed June 22, 2024. https://renaissance.stonybrookmedicine.edu/system/files/EOCReferenceCardsfor2024_.pdf
19. Accessed June 22, 2024. https://www.osha.gov/ionizing-radiation/control-prevention
20. Accessed June 22, 2024. https://www.osha.gov/ionizing-radiation/background
21. Radiation protection guidance for hospital staff – Stanford environmental health & safety. Accessed June 22, 2024. https://ehs.stanford.edu/manual/radiation-protection-guidance-hospital-staff/radiation-exposure-protection
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.
Post a comment