Science Communication Capstone Project: An HPV Vaccine Communication Intervention for Uninsured Gynecology Patients
Introduction
Science Communication Philosophy
I believe that science communication is an inevitable yet underappreciated responsibility of all scientists. In fact, I would assert that scientists need communication skills to be successful, regardless of their field of work or study. Yet, in my training as a medical student and public health scientist, communication has been underemphasized. In order to relay diagnoses and treatment recommendations, health professionals must know how to successfully translate their knowledge into a form that patients can understand. Unfortunately, patient communication skills are briefly touched upon early in medical training but are not re-emphasized at the various stages of medical training, though we know that successful patient communication is an important contributor to health outcomes. As chronic diseases are on the rise and more people must manage these conditions over the long term, communication between providers and patients is becoming even more vital. From medication errors to misunderstanding the seriousness of a prognosis, ineffective communication is a detriment to patients' health. Thus, I am especially motivated to bring awareness to the applications of science communication in healthcare, specifically within patient communication.
An ethical principle that guides my work in science communication is the tenet of patient autonomy. As a healthcare provider, I hope to empower patients to make the best health decisions for their unique circumstances. I aim to guide patients through the decision-making process by listening intently and effectively relaying relevant health information to them. I hope that my patients make good health decisions, but I recognize that I must allow them to come to their own decisions. Therefore, I seek to present all the facts— benefits and risks— to help them weigh their options. I hope to be seen as a resource my patients can utilize to achieve optimal health. I have developed an informative, non-judgmental patient communication style in which I explain my recommendations while maintaining my patients’ autonomy.
Project Overview
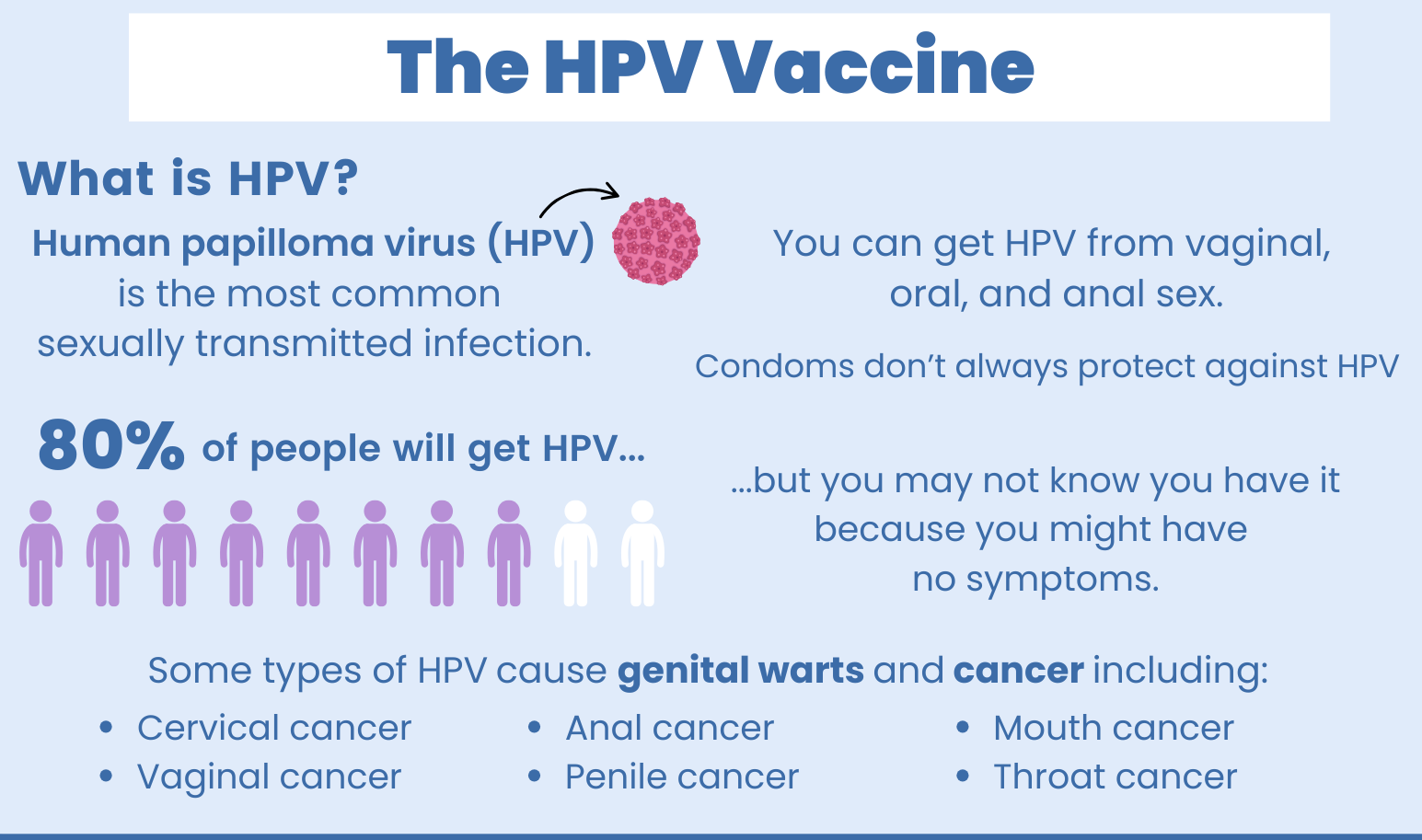
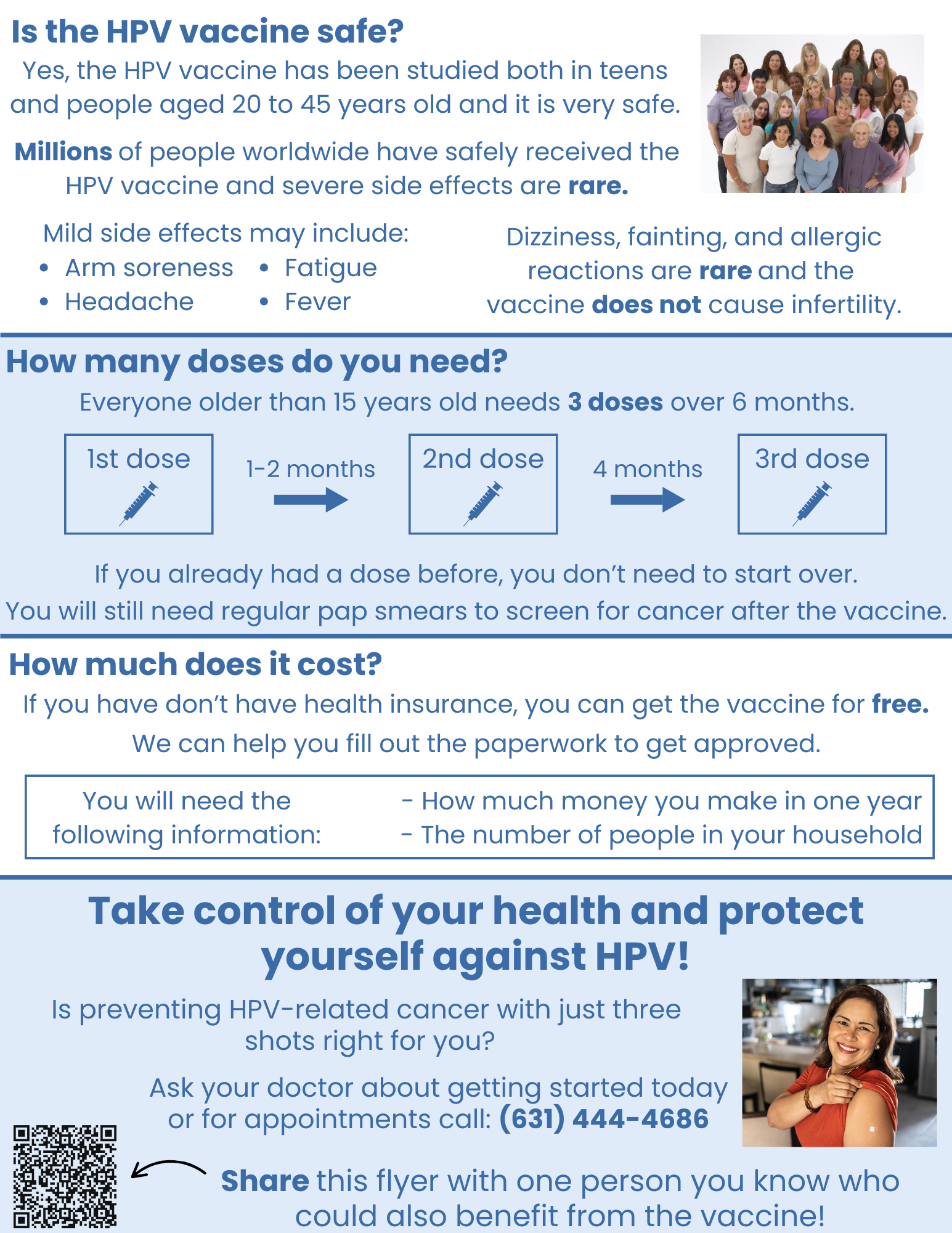
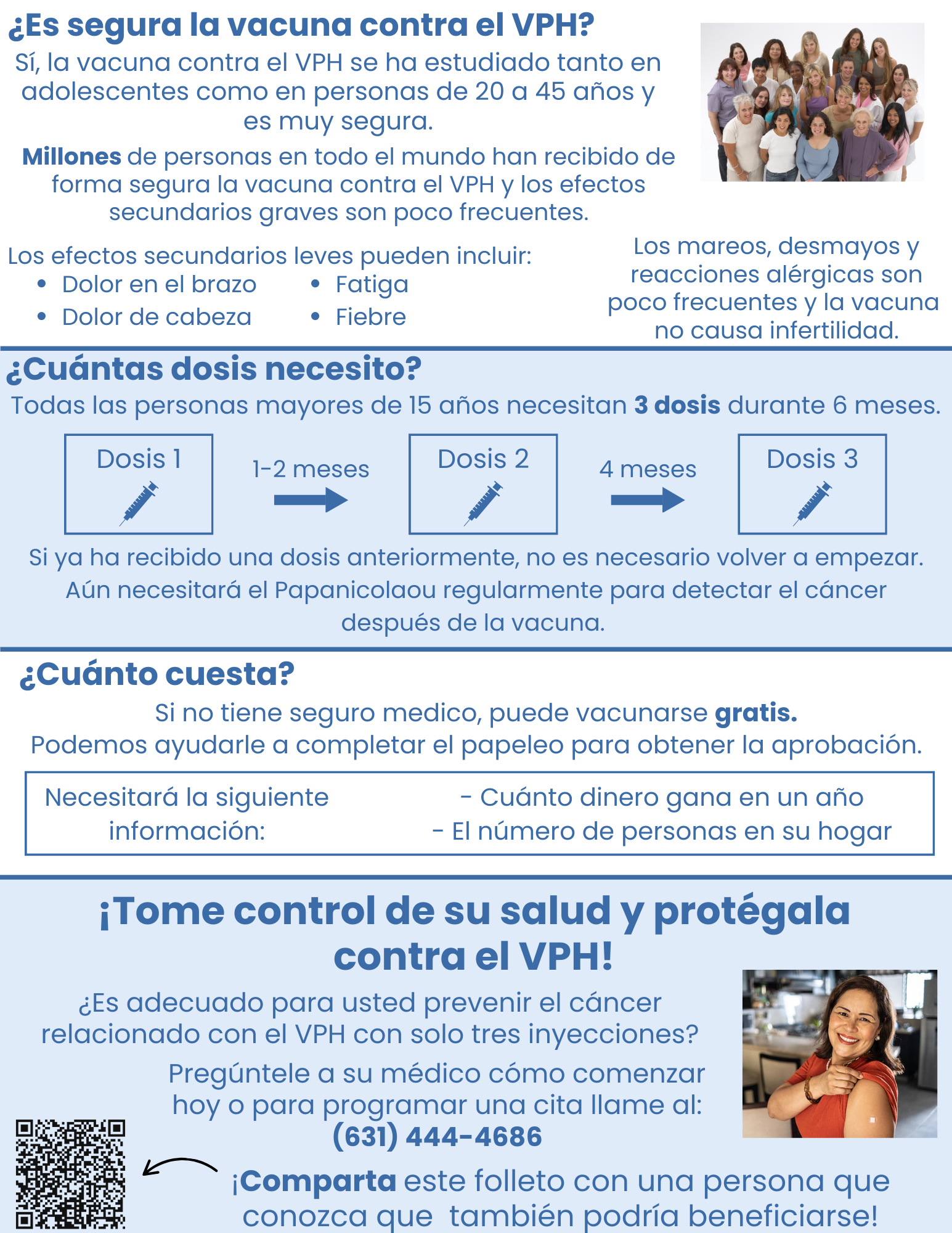
For this project, I chose to create a patient-centered communication intervention to integrate into my ongoing work with uninsured gynecological patients. I sought to create a flyer to aid patients in making an informed decision about the HPV vaccine, Gardasil, to protect against HPV-related cancers. This project aligns with my Science Communication Philosophy, which is centered around improving provider-patient communication, and the ethical principle of patient autonomy that grounds my work. With this intervention, I sought to inform patients about the benefits and risks of the HPV vaccination to empower them with the information they need to make an informed decision.
Project Description
HPV and Vaccination
The HPV vaccination (Gardasil-9) is a three dose series that protects against nine of the most high risk strains of the human papillomavirus associated with cervical, anal, and oral cancers. The vaccine is recommended for all children in early puberty to protect them prior to exposure to the virus. Unfortunately, many patients never received the full three-dose series. Though they have a higher incidence of cervical cancer than the general population, minority, low-income, and uninsured women are less likely to have received Gardasil-9 (CDC, 2024; KFF, 2024). Data demonstrates a higher-than-expected incidence of HPV among uninsured populations. Therefore, this project sought to promote the Gardasil-9 vaccine specifically to a population of uninsured patients.
Access GYN
Access GYN is the resident-run free clinic of the Stony Brook University Hospital Department of Obstetrics and Gynecology, which provides preventative gynecological care to uninsured patients in Suffolk County on Long Island. The clinic administration is currently seeking to increase the number of patients who complete the HPV vaccine (Gardasil-9) series. This project aims to develop and distribute a more accessible HPV vaccine information packet that is specifically targeted to the patients of Access GYN. By creating a patient-centered information packet about the vaccine and its corresponding financial assistance program and integrating it into the clinic workflow, patients will be better equipped to make an informed decision to receive the series.
A significant barrier to increasing HPV vaccination at Access GYN is the lack of time to address the needs of a high volume of patients and also counsel them about the HPV vaccine. The existing patient education materials on the Gardasil-9 are text-heavy and nonspecific to the demographic that Access GYN reaches. Therefore, this intervention sought to improve the quality of vaccine information that is available to patients in the clinic in hopes of better communicating the advantages of HPV vaccination and encouraging patients to receive the shot. Another goal of this project was to integrate this communication intervention into the clinic's workflow. While patient education materials about Gardasil-9 will not replace a conversation with a physician, they may better prepare patients to have an informed conversation with their doctor about the vaccine, helping to streamline the increasing HPV vaccination rates at the clinic. In sum, this communication project attempted to fill a gap in healthcare in which patients are not receiving a potentially life-saving preventative intervention.
Audience Analysis
The intended audience of this project is the subpopulation of SBU Access GYN clinic patients who are eligible for the HPV vaccine but have not yet completed the three-dose vaccine series. The clinic serves uninsured patients from across Suffolk County who are unable to access or afford gynecological care elsewhere. The majority of these patients identify as female. Access patients range in age from 18 to 80 years, but the intended audience of this intervention will be those <46 years old, as they are eligible for the vaccine. This patient population is diverse in its ethnic breakdown, but many identify as Hispanic/Latino and primarily speak Spanish, requiring translators in the clinic. Most come from a low-income background, have limited access to healthcare, and have low levels of health literacy. Based on prior clinic data, Access patients are more likely than the general population to have previously tested positive for an HPV subtype and/or have had abnormal pap smears. A prior history of HPV infection and/or cervical dysplasia underscores the importance of administering the Gardasil vaccine to prevent reinfection with other HPV strains.
We do not know the Access GYN patient population’s baseline knowledge about HPV or their attitudes towards the vaccine. Some may already be familiar with the vaccine and its benefits, while others have heard of it before. Prior knowledge about the HPV vaccine will help facilitate their uptake with the information that will be presented to them. On the other hand, some patients may already be familiar with the vaccine and its purpose. A standard information packet must accommodate those without prior knowledge, so I included the basics about HPV and cervical cancer risk as well as the benefits of the vaccine. Additionally, it is important to keep in mind that some patients may be misinformed about the vaccine and have negative attitudes toward it. These preconceived notions may present a barrier to this communication intervention.
Science Communication Integration
My HPV communication project integrates both the general approach and specific strategies I learned through my previous science communication classes. Most broadly, I use an audience-centered approach throughout the development of the educational materials. Through Foundations of Science Communication, we learned that targeted messages are more likely to be impactful and successful in achieving their goal. As mentioned throughout the audience analysis, I considered the characteristics of my audience and how they may impact my proposed intervention. I also considered how my audience will perceive my message and adjusted accordingly to be most effective in achieving my goals. I turned my audience analysis into specific tactics I employed to design a message for my audience.
In the Communicating Health Risks course, we studied several communication theories that can be employed to understand risk-taking or health-seeking behavior. For instance, the Health Belief Model integrates several variables to consider when developing an intervention to change behavior. Through this intervention, I helped my audience develop accurate perceptions of their susceptibility to HPV infection and the severity of the risk it poses to them. These perceptions create their perceived risk of HPV and cervical cancer. I also demonstrated the benefits of the HPV vaccine, including how it prevents over 90% of all cervical cancers, as well as the perceived barriers, including side effects and costs. I helped patients overcome these barriers by informing them of the safety of the vaccine and the availability of the financial assistance program to provide the vaccine at no cost. Using the Health Belief Model as a framework for communicating HPV risk and promoting vaccination as a preventative measure helped me best communicate with my audience.
I adhered to the design principles we learned in the Foundations course to create the educational packet. The handout was designed to supplement a discussion with a physician about the HPV vaccine, so it contains only the most essential points. At the same time, the document is able to stand on its own. I planned to convey all risk statistics in absolute values rather than relative ones. I also planned to use images and pictographs to convey information when appropriate. Finally, I planned to not overcrowd the documents and make them visually appealing, and use contrast to highlight key messages, and use color and font size strategically.
Project Goals
Audience-centered communication goal: Empower Access GYN patients with the knowledge to make an informed decision about the HPV vaccine through a targeted education intervention
Learning goal: Critically evaluate patient education materials
Learning goal: Communicate health information through visuals and infographics
Learning goal: Modify the patient education packet to be most inclusive of the Access patient population.
Outcome goal: Create and coordinate the distribution of HPV education materials in the form of physical and electronic flyers among the Access patient population.
Outcome goal: Integrate the HPV patient education packet into the clinic workflow.
Outcome goal: Increase the number of patients at Access GYN who are vaccinated against HPV to protect them against HPV-related cancers.
Project Narrative
Reviewed Current HPV Patient Education Materials
First, I conducted research on HPV, HPV vaccination, and previous educational interventions that have been proven to increase vaccination rates. I used these sources to construct an annotated bibliography. Second, I collected existing HPV vaccine materials from sources like the Centers for Disease Control, National Institutes of Health, World Health Organization, UpToDate, the American Cancer Society, and the Mayo Clinic. I made note of the communication strategies they employed and highlighted important information I should include in my flyer.
Outlined and Constructed Flyer
I used the material from the annotated bibliography and my analysis of the current education materials to create a basic structure for the patient education packet. First, I translated the content I put in my outline into patient-friendly language on a blank document. I organized it in sections with different question-based headings. Next, I experimented with different design themes, colors, layouts, and fonts in Canva. I created a simple theme with good color contrast to make the text pop. I experimented with different font sizes and bold text. I also added different pictures and graphics to make the flyer more interesting and engaging. I was able to narrow down all of my content to two pages that will be in a front and back flyer.
Revisions
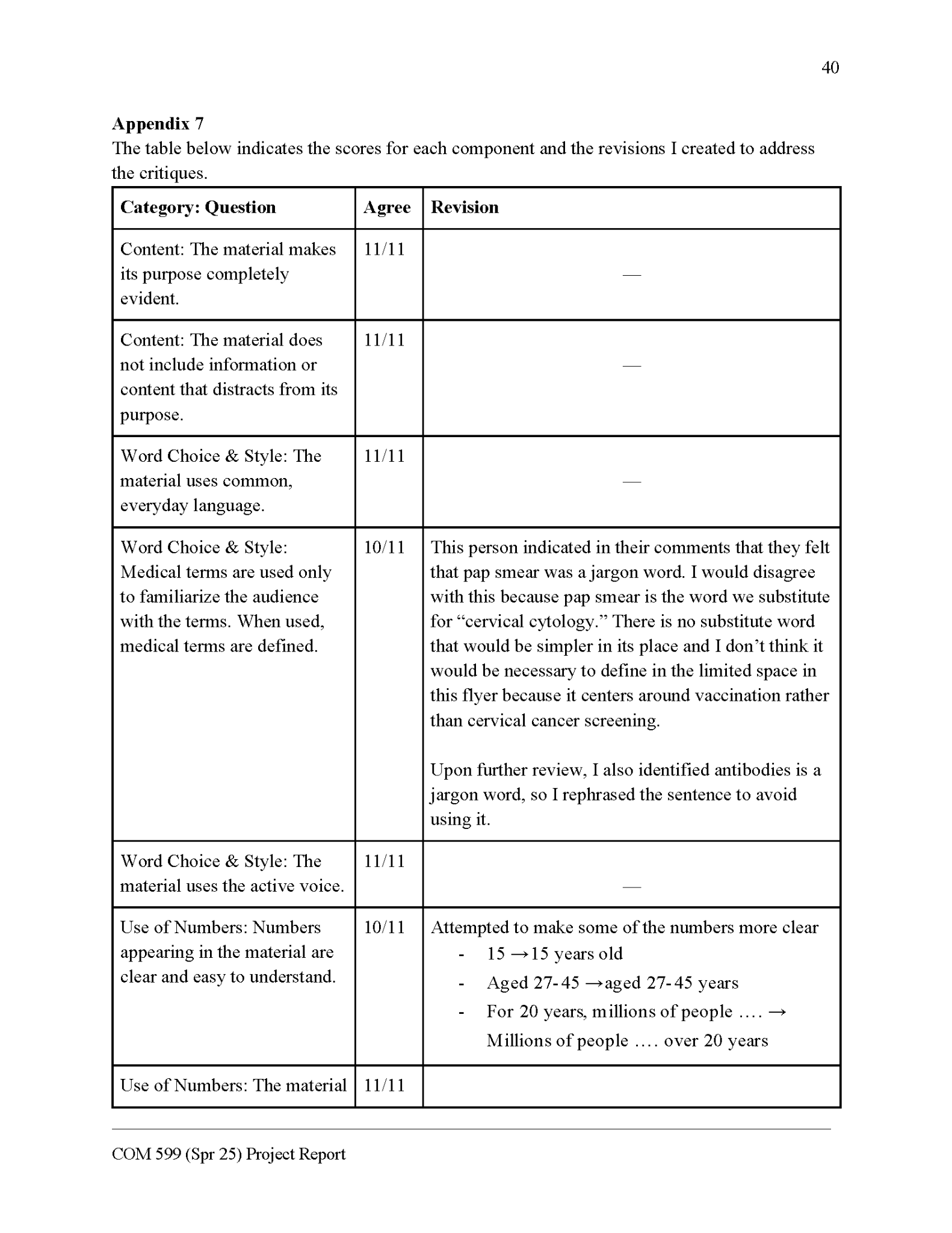
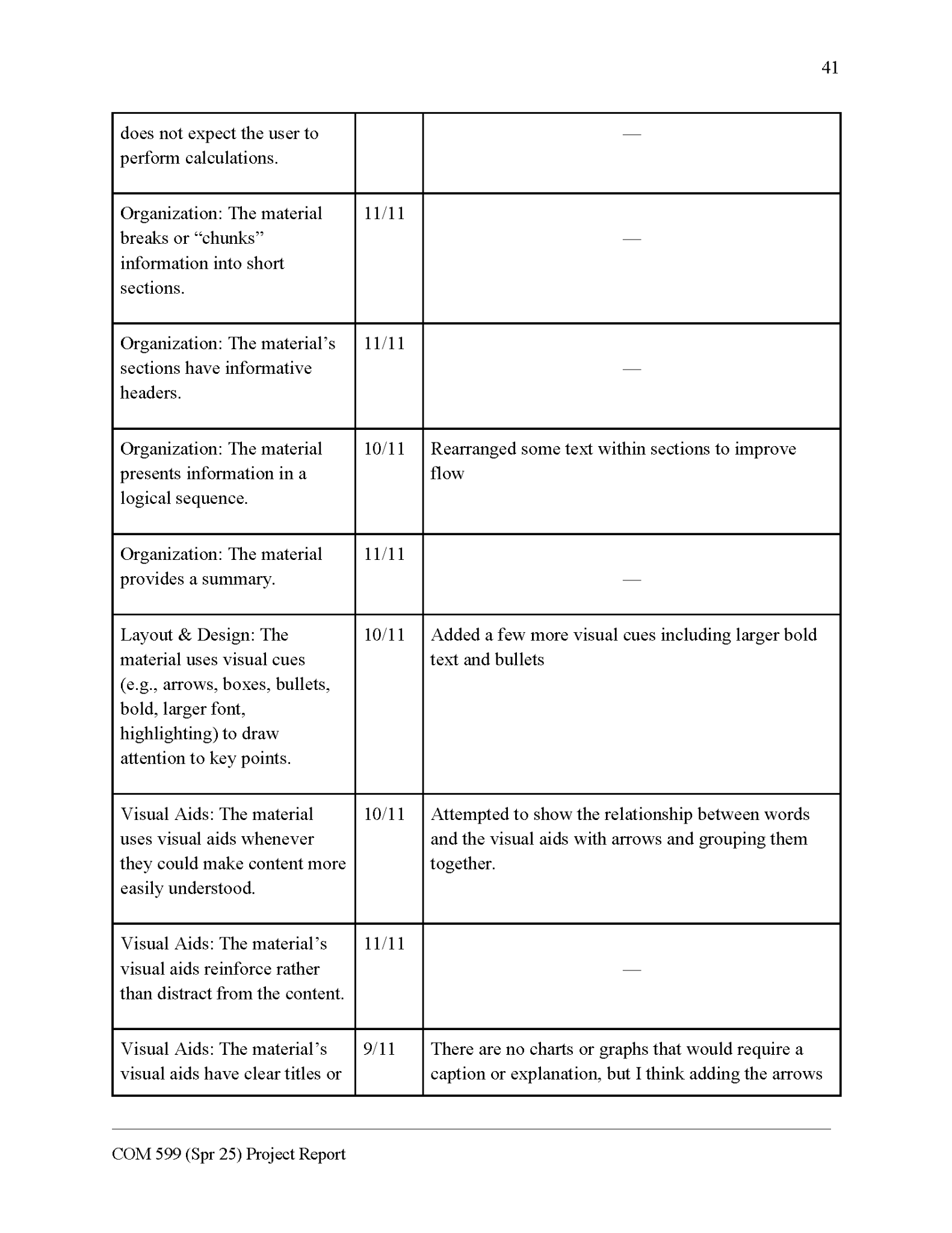
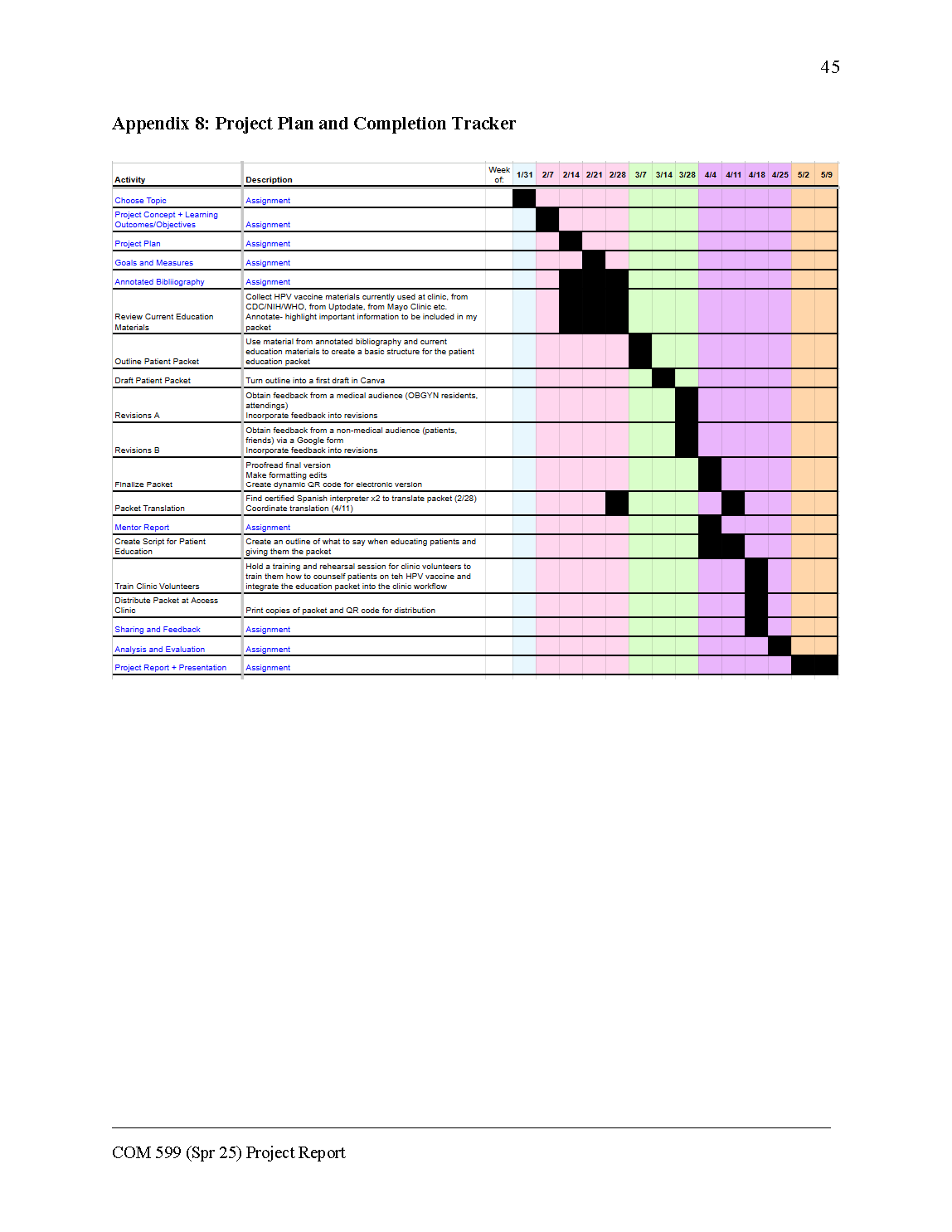
I went through two types of feedback. First, I obtained feedback from a medical audience (OBGYN residents and attendings) on the medical content of the flyer and any suggestions they had for revisions. Next, I obtained feedback from a non-medical audience (patients, friends) via a Google form that incorporated the Patient Education Materials Assessment Tool (PEMAT). This derived a score for my flyer based on the content, word choice and style, use of numbers, organization, layout and design, visual aids, and actionability. I then proofread the finalized flyer and made formatting edits. I recruited certified medical Spanish interpreters to translate the flyer and coordinated with them the translation of the flyer. I then formatted the translation into the Canva template for the flyer.
Created Provider Training
Next, I created a provider training, which consisted of an outline of what to discuss with providers as well as a tip sheet for them to remember the key points. I essentially distilled my outline of HPV information and the strategies of successful HPV vaccine education campaigns into a list of short bullets for them to look over before they counsel patients. I planned to conduct the training at the start of the clinic day, before the patients arrive. The training also included a rough script for me to explain my intervention and how to use it successfully. I also included a few training activities, such as questions and role play, to help the providers practice and develop their recommendations.
Trained Clinic Volunteers and Distributed Flyers
First, on the morning of Wednesday, April 16th, at the Access GYN clinic, I held the training and rehearsal session for clinic volunteers to train them how to counsel patients on the HPV vaccine and integrate the education packet into the clinic workflow. I talked to them for approximately 15 minutes about using the flyer, and we went through a few of the practice scenarios. I elicited their feedback on the training. I also coordinated the distribution of the HPV flyer to eligible patients at the clinic. The resident assigned to see each patient was responsible for discussing the flyer with them.
Deliverables
HPV Vaccine Flyers - English and Spanish
Please see Appendices 3 and 4 for the finalized version of the flyers.
Feedback
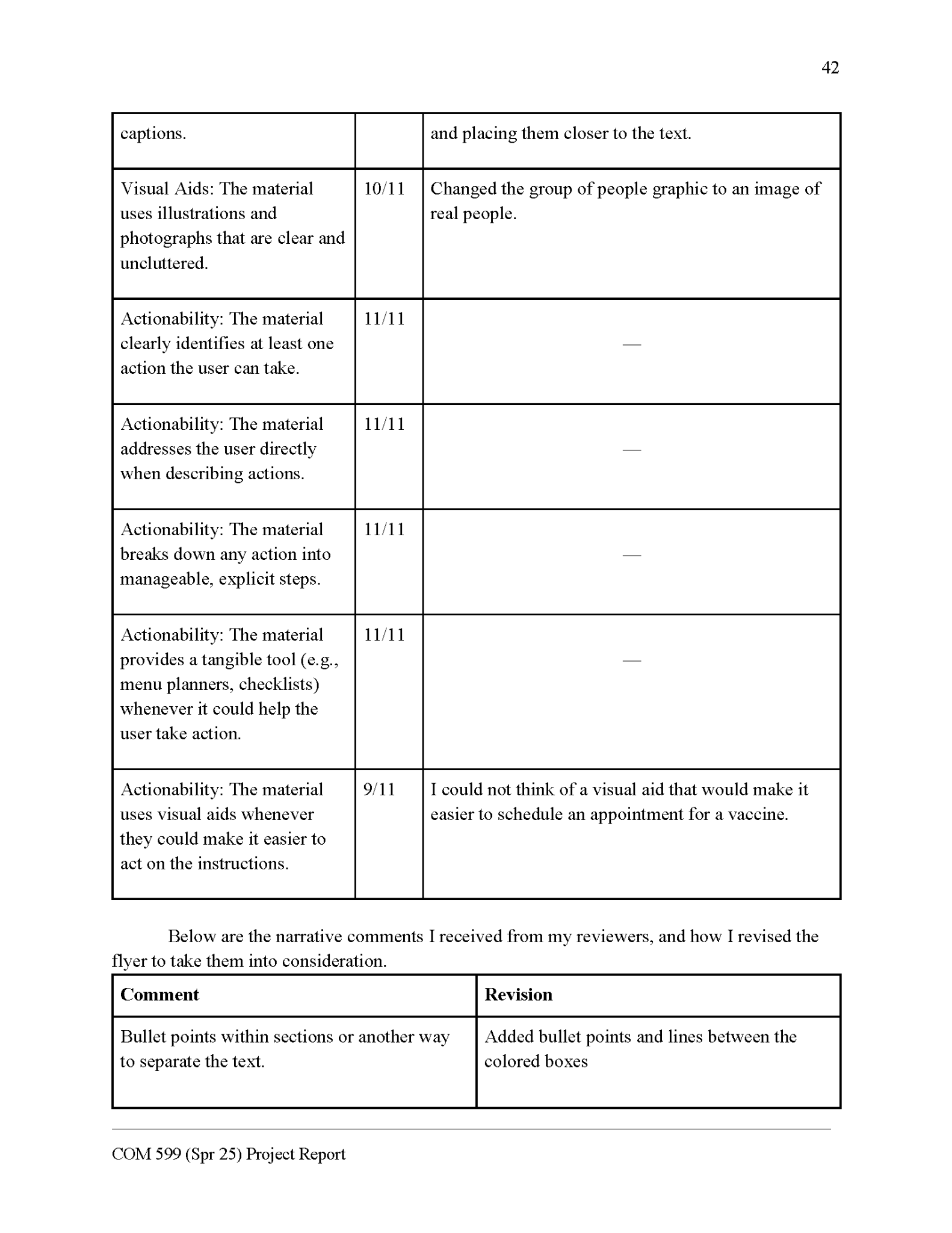
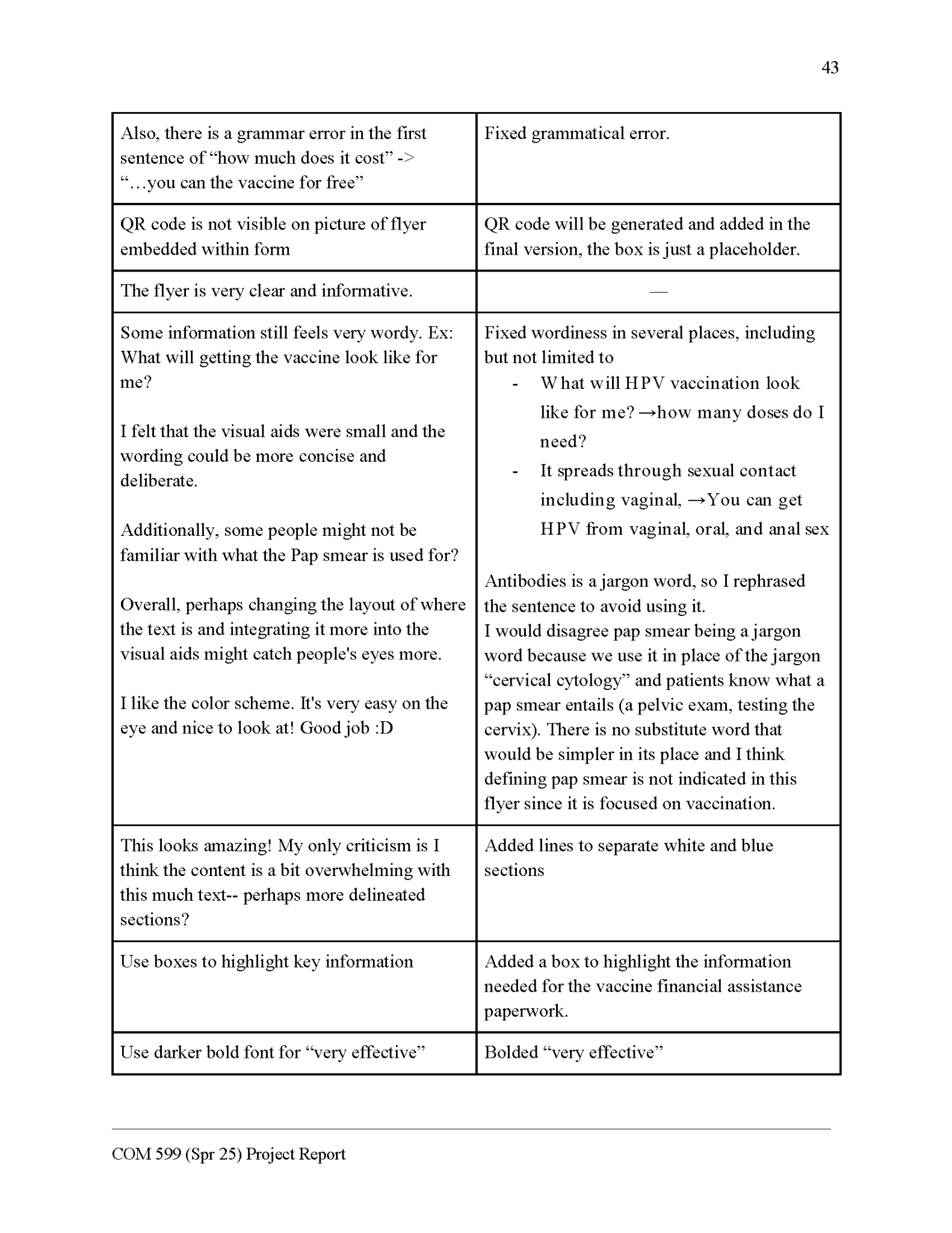
The average PEMAT score for my flyer from my nonmedical reviewers was 20.09/21. This high average score indicates that most participants indicated through the PEMAT that my flyer was on target. Please see Appendix 7 for a breakdown of the feedback I received and how I responded to that feedback.
Provider Training
Please see Appendices 5 and 6 for a copy of the provider training and tip sheet.
Project Analysis
Learning Goal: Critically evaluate patient education materials
I reviewed a large number of existing HPV vaccine patient education materials and devoted a lot of time to this planning part of the process. I think that this effort made my flyer even stronger. During the review process, I identified more than my goal of five successful strategies and three unsuccessful elements common to these materials. Overall, I identified several common themes and strategies used in prior education materials that help me generate ideas about what to include in my own flyer.
Learning Goal: Effectively communicate health information through visuals and infographics (evaluation from at least 10 nonmedical reviewers and five medical reviewers)
I reached my goal of having 10 nonmedical reviewers complete the PEMAT and five medical reviewers comment on the flyer. I received very useful feedback that I was able to use to revise my flyer. The high average PEMAT score of 20/21 for my flyer indicated that I was successful at developing a patient-centered communication tool. The commentary feedback helped me identify and eliminate jargon words, make the phrasing more concise, and improve the visual organization of the flyer. These improvements based on the feedback helped me better communicate my message about the HPV vaccine through the flyer.
Audience Centered Goal: Empower Access GYN patients with knowledge to make an informed decision about the HPV vaccine.
The flyer was used to help counsel patients on the HPV vaccine at the monthly Access GYN clinic on April 19th, allowing them to make a more informed decision about whether it would be the right decision for them. Four of six eligible patients received the flyer and counseling on this day, which is fewer than I had aimed for. I anticipate that this was because it was the first day of integrating the flyer into an already busy clinic. I am hopeful that we will continue to empower patients with this information to enable them to make an informed decision about the HPV vaccine in the coming clinic days. I will continue to work towards this goal by integrating the flyer into future Access GYN clinic days.
Audience Centered Goal: Modify the flyer to be most inclusive of the Access patient population.
I made my flyer inclusive of the patient population at Access GYN by customizing the information and format to be accessible to the clinic’s primarily Spanish-speaking population of uninsured patients. Specifically, I used no greater than a 6th-grade reading level, coordinated a Spanish translation, using inclusive images, and addressed the concern about the HPV vaccine cost in the flyer. These characteristics align with the majority of the Access GYN patient population being Spanish-speaking, uninsured patients. I believe that this customization helped patients feel that this communication was centered around them.
Outcome Goal: Coordinate distribution of education materials in the form of physical flyers among the Access patient population (at least 10 flyer copies [modified to account for the fact that only one clinic day would occur in the time frame])
As mentioned, four of six eligible patients were given the flyer when they were counseled by their physician at the 4/16 Access GYN clinic. This means that two HPV vaccine-eligible patients did not receive the flyer. This gap was due to logistical issues and timing of the clinic day; we did not have a medical student volunteer helping the resident with the patients, and we had to keep the clinic moving since all patients were there for issues other than the vaccine. This was also a lighter clinic day, so there were fewer than the estimated 10 eligible patients per clinic day that I had anticipated. As we integrate the flyer and training into the clinic, I believe that we will increase the average number of HPV vaccine flyers distributed during each clinic day.
Outcome Goal: Coordinate the distribution of education materials electronically among the Access patient population (at least 5 QR code views [modified to account for the fact that only one clinic day would occur in the time frame])
There were three views of the electronic version of the Spanish version of the flyer from the dynamic QR code after the 4/16 clinic day. While this fell short of my adjusted goal of 5 QR code views, I believe that I will be able to reach this target as I improve the implementation of the flyer and its integration into the clinic workflow. No copies of the English version of the flyer were distributed to Access GYN patients at the 4/16 clinic, so it makes sense that there were no views of the electronic version of the English flyer.
Outcome Goal: Integrate patient education packet into clinic workflow through provider training (at least two residents and at least five medical students)
I met my goal of piloting the training with at least two residents at the 4/16 Access GYN clinic. They offered me feedback on the training and expressed their concerns about the flyer and the HPV vaccine initiative. I was able to address their concerns about having enough time to integrate the flyer into the clinic workflow by deciding to recruit a medical student to specifically help with this each clinic day. I was not able to hold training for medical students due to time constraints. The third-year medical students whom I would be recruiting and training use the HPV vaccine flyer at Access GYN are currently in the final study phase in preparation for an important exam, so I recognized that I would likely not be able to recruit them for training before the course ended. I postponed this training to a later date and instead focused on editing the training script and tip sheet I developed based on the feedback from the residents.
Outcome goal: Increase the number of patients at Access GYN who get at least one dose of the Gardasil vaccine (at least five on 4/16/2025)
I fell short of my goal of at least five vaccinations, as only two of the four patients who received the flyer were vaccinated against HPV on the day of the clinic. However, the additional two patients who were counseled are scheduled to come back for the vaccine at a later clinic day. This brings the total of patients who were connected to HPV vaccination on this day to four, which is not far off from my goal of five. This was the first day that this program was introduced into the clinic, so nonetheless, I think two vaccinations on that day is a great start. As we integrate the flyer and training into the clinic, I anticipate that we will increase the average number of patients vaccinated each clinic day.
Future Directions
This project is just a starting point for my work with HPV vaccine communication. I am planning to continue to incorporate the flyer into clinic days as I continue my work with the monthly Access GYN clinic. I will again distribute the flyer on the 5/21 clinic day, using what I learned from the first implementation day to be more successful. I hope that with each clinic, we are able to find a more consistent workflow that allows us to meet all of our patients' needs and counsel them on the HPV vaccine.
There are some specific components I would like to continue working on in the coming months. I will be training more residents to use the flyer, and will begin a phase of training medical students too, as I did not have time to start this component during this course. I also think it would be valuable to get patient feedback on the flyer, as the goal is to serve their needs. I hope that asking the patients their opinions on the HPV vaccine flyer will be further evidence that my intervention was successful. If patients have any concerns about the flyer, I will be receptive to their feedback and incorporate it into another revision of the flyer.
Finally, I am looking forward to the possibility of sharing the resources I made with other similar clinics so a larger audience may benefit from them. I will need to investigate this option more and determine how to contact other gynecological clinics for uninsured patients. I hope to discuss my project at an upcoming conference and potentially make connections there to help disseminate my flyer to a wider audience.
Conclusion
In sum, I created and implemented a successful HPV vaccine communication program through the creation of a customized flyer specific to the Access GYN patient population. I fell short of some of my goals, but they were rather ambitious considering I only had the first clinic day to achieve them. I anticipate that this project will continue to grow as I continue to work with Access GYN to promote the HPV vaccine to eligible patients.
This project greatly contributed to my development as a science communicator. I practically applied the knowledge and skills that I have garnered throughout my certificate program to make a meaningful change in my community. I further developed my design skills and learned to be receptive to feedback on my work by going through a revision process. I anticipate that this project will only grow as I further develop my skills as a science communicator and continue to implement my HPV vaccine flyer into the Access GYN workflow.
I will also continue to grow as a science communicator through my commitment to a lifelong journey of learning and practice. I plan to build upon my knowledge base as I aspire to be a more successful science communicator each day. This growth will be an active process throughout my career as I keep abreast of the latest research, hone my skills, and help other scientists reach their communication goals. I want to inspire more health professionals to become excited about science communication so we can communicate our work more effectively, enabling us to have a greater impact.
Appendix 1: Annotated Bibliography
HPV Vaccine Background: Benefits and Safety
KFF: The HPV Vaccine: Access and Use in the U.S.
This contains general information about cervical cancer epidemiology and screening, including background on HPV, cervical cancer incidence rates, and screening rates, as well as disparities by race, socioeconomic status, and insurance coverage.
This background information is mostly a review for me, but ensuring I have a solid understanding of HPV and cervical cancer will be important as it will inform my further research. Some of this data can also help me demonstrate the need for HPV vaccination among the Access population, which serves a large percentage of uninsured women and Hispanic women.
- ● HPV is the most common STI
- ● There are more than 200 known strains of HPV
- ● Racial disparities in cervical cancer incidence and mortality rates
- ○ Hispanic women- highest incidence rate, but mortality rates are comparable to the national mortality rate.
- ○ Black women – third highest incidence rate, yet highest mortality rates
The HPV vaccine has an excellent safety profile and is similarly well tolerated between women 16–26 years of age and women 27–45 years of age, according to this phase 3 study comparing outcomes in the two groups.
This safety information specific to the older population of women will be important to convey in my patient education packet to demonstrate that the risks of HPV vaccination are much less than the benefits, specifically for the population of patients that Access GYN serves.
- ● “The most common injection-site AEs were pain, swelling, and erythema, which occurred in 86.1%, 23.3%, and 19.5% of women aged 16–26 years, and 82.8%, 23.3%, and 16.9% of women aged 27–45 years, respectively.”
- ○ Most were mild or moderate in intensity
Describes the rates of HSIL + and the rates specifically among women older than the typical age of HPV vaccination. This population makes up nearly half of all cases.
This information will help support my argument that HPV vaccination is important in women outside of the adolescent age group because nearly half of all cases are due to vaccine-covered HPV types in women >30.
- ● “Approximately 196,000 cases of high-grade cervical dysplasia were diagnosed in the United States in 2016”
- ○ “97,000 were diagnosed in women ≥30 years of age and attributable to HPV types targeted by the 9vHPV vaccine”
HPV vaccination has decreased the rates of HPV infection and high grade cervical dysplasia, based on the results of a systematic review and meta-analysis. The impact of the vaccine is greater in countries that attempt to vaccinate more than just adolescents.
This will help me emphasize the benefits of the HPV vaccine to my patient population of women outside of adolescence.
- ● “A systematic review and meta-analysis of the population-level impact of vaccinating girls and women against human papillomavirus on HPV infections, anogenital wart diagnosis, and cervical intraepithelial neoplasia grade 2+ (CIN2+)”
- ● There is strong evidence of HPV vaccination successfully preventing cervical cancer
- ○ Both the high-risk HPV infection and CIN2+ are significantly declining
HPV Vaccination Rates
Over half of young adults had ever received at least one dose of the HPV vaccine. Hispanic adults are much less likely to have received any dose of the HPV vaccine..
This demonstrates the need for intervention to increase HPV vaccination rates among Hispanic young women especially, since they lag behind compared to the overall average. This population is one that Access GYN serves, so this will help inform my intervention.
- ● Overall, in 2019, 47.0% of adults aged 18–26 years had ever received any HPV vaccine
- ● “Non-Hispanic White adults (49.7%) were more likely than Hispanic adults (40.6%) to have ever received an HPV vaccination; differences between non-Hispanic Black adults (45.8%) and the other two groups were not statistically significant”
In a study of older women eligible for the HPV vaccine, Hispanic women were less likely to have received the vaccine.
This source further supports that Hispanic women, especially adults, are less likely than other groups to have been vaccinated for HPV. This helps support my intervention geared towards a cohort of patients that are predominately in their late 20s through early 40s and Hispanic.
- ● Compared to white adults between 27 and 45 years, Non-Hispanic Black adults were more likely to have been vaccinated against HPV but Hispanic adults were less likely to have been vaccinated
- ○ A previous study of adult Hispanic men and women conducted prior to the updated expanded age of eligibility in 2018 found no significant difference
Human Papillomavirus Vaccination Among Young Adults Before and During the COVID-19 Pandemic
HPV vaccination rates were increasing pre-pandemic, but they have stagnated since. There are also education and socioeconomic status disparities in HPV vaccination rates, such that those with less education and lower income are less likely to have received the vaccine series.
This information adds support to my project’s aim of increasing vaccination rates specifically among women who are uninsured and have less education, which is the patient population that Access GYN serves..
- ● “Unlike the increase in HPV vaccination rate from 2018 to 2019 (39.9% to 47.0%; P < .001), no significant change was observed from 2019 to 2022”
- ● Coverage was lower among uninsured males and females
- ○ Higher among higher education
Awareness and Knowledge of HPV Vaccination
Awareness and knowledge of HPV and HPV vaccination among adults ages 27–45 years
Most participants were aware of HPV and its association with cervical cancer, but fewer understand its link to other cancer types. Those who were more knowledgeable about HPV tended to be those with higher education. The findings also suggest that the socioeconomic differences in HPV knowledge may exacerbate existing disparities in vaccine uptake.
This assessment gives me a baseline understanding of the current state of knowledge of HPV vaccination among women at the higher end of the eligibility window. Understanding what typical patients know and don’t know about HPV and its vaccine will be essential in developing my educational content that is intended to be geared towards Access GYN patients.
- ● 80% of people will get HPV
- ● Oncogenic strains → 34,800 cases of cervical, anal, penile, vaginal, vulvar, and oropharyngeal cancers annually in the United States
- ● “In 2018, the FDA approved HPV vaccination for people ages 27–45 According to the National Health Interview Survey 2017, 15.8% of women and 3.2% of men ages 27-to-45 years old had received at least one dose of the HPV vaccine”
- ● Health Information National Trends Survey (HINTS) is sponsored by the National Cancer Institute (NCI)
- ● A majority of respondents were aware of HPV (72.9%)
- ○ Female sex, college educated
US born Latinas and Latina immigrants are less likely to be informed about the HPV vaccine and know less about where they can find more information about it. This knowledge gap may exacerbate disparities in HPV vaccination uptake.
This is important to know for my project because many Access GYN patients are recent immigrants, and thus may have a lower baseline understanding of HPV. Keeping in mind that my audience may have a lower knowledge base on my topic will be essential when developing my education materials.
- ● Compared to US born Americans, immigrants were less informed about vaccine availability and accessibility
- ● Compared to US born Latinas, Latina immigrants were less likely to have heard of HPV vaccine and know where they can get more information about HPV vaccine
Young women aged 27-45 are less likely to know that they are eligible for HPV vaccination, and most were under the impression that it was something just for teenagers. Many didn’t think that the vaccine would offer them any protection at this point in their sexual lives. This study also identified this age group’s concerns about the HPV vaccine had to do with safety specifically for their age group.
This information is important because it shows that it will be essential that I correct patients’ misunderstanding about their eligibility for HPV and the utility of the vaccine for people of their age. Knowing this age group's concerns about HPV vaccination is also important because they do not align with the concerns of the parents of the younger population that the vaccine is typically marketed for. This study also informs me that the main concerns adults have about the HPV for themselves are the safety and the utility of the vaccine. These will be concerns that I should address in my patient education packet.
- ● Qualitative study
- ○ Knowledge about HPV varied widely
This study also examined knowledge of HPV vaccination and its associated cancers. It found that baseline knowledge was lower among those who identified as Hispanic and those with a lower level of education. They also identified that many people believe that HPV is not sexually transmitted.
These results will inform my education intervention similarly to a previous study that found that certain subsets of patients have a lower baseline knowledge of HPV vaccination, but also lower knowledge about HPV itself. I will thus provide a brief overview of what HPV is before I talk about the benefits of vaccination against it when I develop my education materials.
- ● “Hispanics (OR=0.50, 95% CI=0.30, 0.82) and those in the “other race” race category (OR=0.36, 95% CI=0.17, 0.75) were significantly less likely to have heard of the vaccine compared to whites, as were those with a high school degree compared to those with a college education”
- ● “A little over half of Americans (55.7%) knew that HPV is an STD, 31% were unsure, and 20% inaccurately believed that it is not an STD”
Strategies and Predictors of HPV Vaccine Uptake
The gaps in adolescent awareness of HPV vaccination are due to a lack of knowledge and misinformation of their parents. Many interventions have been successful in increasing adolescent HPV vaccination rates. These include early discussion prior to eligibility and educational interventions addressed at the parents.
My audience contrasts from an adolescent audience because they are older and thus able to make their own health decisions. Therefore, interventions that increase adolescent vaccination will likely not have fidelity when applied to a new age group. However, these prior interventions can also help inform the educational intervention I am developing to some extent.
- ● Adolescent HPV vaccine uptake ~75% in 2020
- ○ Below Healthy People 2020 goal of 80%
Provider communication and HPV vaccination: The impact of recommendation quality
This study highlights research demonstrating that provider recommendation increases the odds that a child or adolescent patient will both initiate and complete the HPV vaccine series. Additionally, the higher the quality of the recommendation, the higher the likelihood of receiving at least one dose.
While this study involved HPV vaccination of adolescents, it still informs my education intervention. It demonstrates that the quality provider recommendation makes a substantial difference in vaccine outcomes. This data supports my project and may aim to use the patient education packet to help providers deliver higher quality counseling and recommendations regarding the HPV vaccine. I will ensure that providers are adequately trained in discussing the HPV vaccine with patients through a training session.
- ● Among adolescents, higher recommendation quality correlated with HPV vaccine initiation
- ● “In terms of overall quality, receiving a high-quality recommendation versus no recommendation was associated with over nine times the odds of having received at least one dose of HPV vaccine (23% versus 74%, odds ratio [OR]=9.31, 95% confidence interval [CI], 7.10–12.22)”
- ○ Receiving a low-quality recommendation versus no recommendation was associated with over four times the odds of initiation
Health Literacy Correlates to HPV Vaccination Among US Adults Ages 27–45
This work also substantiates the link between provider recommendation and increased HPV vaccination rates. They recommend using the dimensions of health literacy during an HPV vaccine intervention to ensure that patients not only have access to information about the vaccine, but know how to apply that information.
I can use the fact that this study found that perceived vulnerability to cancer was a significant predictor of HPV vaccination to inform my patient education materials. I will make sure patients understand their risk of cervical cancer and how it compares to the risk after they’ve been vaccinated, which should help motivate them to agree to vaccination.
- ● The dimensions of health literacy can serve as targets for HPV vaccine intervention among adults 27–45 years
- ○ They are (1) access and obtain, (2) understand, (3) process and appraise, and (4) apply and use relevant health information
HPV catch-up vaccination among a community sample of young adult women
This research demonstrates that among the catch-up HPV vaccine eligible population, the strongest predictors of vaccine initiation were perceived peer approval, perceived susceptibility to acquiring HPV, and belief that the vaccine is effective.
I will ensure that I convey patients’ suspicions to HPV and the effectiveness of the vaccine in preventing HPV in my patient education materials because these characteristics were shown to be the most important influences on whether patients in the catch-up population receive the vaccine.
- ● Half of women believed their peers approved of the vaccine
- ● Most (82%) believed HPV would be bad to some degree for their health
- ● Despite this, 70% of women felt low susceptibility to acquiring HPV
- ● Only 25% believed the vaccine was highly effective
- ● “Vaccine initiation was significantly associated with peer approval of the vaccine, perceived susceptibility to acquiring HPV, and beliefs about vaccine effectiveness (p ≤ 0.01 for all), but not with concerns about severity of HPV infection”
- ● Only 19% had initiated HPV catch-up vaccination, and only half of the initiators had completed the 3-dose series, making overall vaccine completion ~10%
Barriers to human papillomavirus (HPV) vaccination among young adults, aged 18–35
This research demonstrates barriers to HPV vaccine among the adult population. They found that most adults did not have an intention to get the HPV vaccine. The most common reasons for this were that they believed the vaccine was not necessary for them and was not safe. Variables that predicted negative intention to get the HPV vaccine included were its cost and not knowing where to get it.
In my patient education materials, I will attempt to address the barriers to HPV vaccination that were identified in this study. I will attempt to demonstrate how the vaccine is necessary in the adult population and support that it is safe. I will also present information on the free vaccination program so the cost is not a barrier for Access GYN patients.
- ● Most young adults aged 18-35 (57.1%) reported they were not at all likely to get vaccinated for HPV in the future 6 months
- ● Lower intent was associated with belief that the vaccine is not necessary and not safe
- ● Targeted programs and policies are needed to increase HPV vaccination among eligible adults, not just adolescents
- ○ Unlike with adolescents, young adults make their own healthcare decisions
- ■ Messages that were effective with parents may not resonate with young adults
- ● Need to adopt them
This study examined what patients need before they thought that they would agree to get the HPV vaccine. Most respondents said they wanted more information about the efficacy of the vaccine. They also found that the vast majority of patients preferred talking with their healthcare provider to get the information they were missing. They also said that information pamphlets were an important tool to aid them in their learning.
This evidence supports my intervention of combining a healthcare provider recommendation with an educational pamphlet to give patients the knowledge and efficacy information they need to make an informed decision about the HPV vaccine.
- ● Many respondents said they did not have enough information about the HPV vaccine to make a decision
- ● Many said that they needed more information about HPV vaccine efficacy
- ● “Preferred information sources regarding HPV vaccination varied, with 87.8% identifying a healthcare professional as the preferred source, to just 36.7% identifying a friend”
- ● “A significantly larger percent (p < 0.05) of respondents with a "shared focus" role in decision making identified healthcare professionals (92.5%), information pamphlets (71.7%), and websites (78.3%) as preferred information sources”
- ● “After healthcare professionals, those with a self-focused decision-making role identified websites (68.3%) and information pamphlets (57.6%) as preferred information sources, whereas respondents with a provider-focused role identified information pamphlets (52.9%)”
CDC: Five Ways to Boost Vaccination Rates
This CDC page provides five tips for increasing HPV vaccination rates and how to implement them in the medical office setting.
I will integrate these into my HPV vaccination education program. While there is no opportunity to bundle vaccinations since only the HPV vaccine is given in this clinic, I will ensure that every patient is reminded about the opportunity to be vaccinated at each visit. We will distribute the education packet to patients at initial visits, annual visits, and follow up visits. I will also prepare answers to common patient questions as part of the patient counseling script that I will give to providers.
- ● Bundle the HPV vaccine recommendation with other vaccines
- ● Ensure a consistent message is given by all members of the office staff
- ● Use every opportunity to vaccinate
- ● Provide personal examples
- ● Be prepared to answer questions
Resources for Creating Materials
The Patient Education Materials Assessment Tool (PEMAT) and User’s Guide
This is a 26 item tool for evaluating patient education materials. It is used to evaluate understability and actionability, and derive a score on the quality of the materials.
I will use this guide to evaluate and revise my patient education materials. I will fill out the PEMAT first as a measure of self evaluation for my own editing. I will also ask my non-medical pilot testers to fill out the PEMAT as well, and take into consideration their input when revising.
- ● Agency for Healthcare Research and Quality
- ● The Patient Education Materials Assessment Tool (PEMAT) is a systematic method to evaluate and compare the understandability and actionability of patient education materials.
- ● Sum points, divide sum by total possible points, multiply by 100
- ○ Each item is worth one point
- ○ 26 total items
This is a list of commonly used complex words and phrases and plain language substitutions. It is part of the Health Literacy Universal Precautions Toolkit from the Agency for Healthcare Research and Quality. They point out that even if patients know what these words mean, using simpler versions will make reading and understanding something less effortful.
I plan to consult this list when I am developing my patient education packet. I am pretty good at replacing medical jargon and terminology when I write, but sometimes I do use more complex language. The patient education packet will be more accessible to patients if I consult this guide to make the language less complex.
Excerpt:
|
Instead of |
Try |
|
absence, absence of |
no, none, not here, not present, without |
|
accessible |
open, ready, within reach, can be used by |
|
accommodate |
meet, agree to |
|
accompany |
go with, show up with, go along with |
|
accomplish |
carry out, do |
CMS Guidelines for effective writing
This is the Center for Medicare and Medicaid Services website for Guidelines for Effective Writing. They give recommendations for content, length, language to avoid,organization, and headings.
I will use this to help me organize my patient education materials and use strategies that are proven to make the most effective materials.
- ● Keep content meaningful & user-focused
- ○ Get to the point, delete the fluff
- ○ Show, don’t tell
CDC: HPV Educational Tools and Resources
This page contains two infographics developed by the CDC to help inform providers how to discuss the HPV vaccine with patients and how to make their interventions most successful. These are specifically targeted towards providers who are planning to talk to parents of eligible children.
These resources will help inform my patient education materials, but also the medical student and provider training on how to counsel patients about the HPV vaccine using the packet. Although these resources are intended for parents, slight modification of these tips can make them appropriate for an adult population eligible for the HPV vaccine.
- ● Top 10 Tips for HPV Vaccination Success (selected)
- ○ Motivate your team and encourage their immunization conversations with parents
- ○ Implement systems to ensure you never miss an opportunity to vaccinate
- ○ Implement systems to ensure you never miss an opportunity to vaccinate.
ACOG: What I Tell Every Patient About the HPV Vaccine
This article provides the perspective of one OBGYN on the best ways to talk about the HPV vaccine with every patient. She gives four tips incated below.
This perspective will help me develop the training for medical students and residents on how to best counsel patients about the HPV vaccine.
- ● “The vaccine is very, very effective”
- ● The vaccine is safe – and important for public health
- ● The vaccine is best for children, but adults can get it too.
- ● The vaccine is still helpful even if you have already tested positive for HPV or have been sexually active for a while.
Existing Patient Education Materials
Uptodate: Patient education: Human papillomavirus (HPV) vaccine (The Basics)
- ● Positive
- ○ Q/A format
- ○ Specified risk with specific sexual activities (vaginal, oral, anal), not just “sex”
Uptodate: Patient education: Human papillomavirus (HPV) vaccine (Beyond the Basics)
- ● Positive
- ○ Q/A format
- ○ Discusses high risk vs low risk subtypes
- ○ Condoms not 100%
Merck: Patient Information about GARDASIL®9
- ● Positive
- ○ Uses bulleted lists
- ○ Contraindications
- ○ Signs of allergic reaction
- ● Positive
- ○ Quantifies years and doses to demonstrate safety
- ○ Emphasizes continued monitoring
- ○ Quantifies risk reduction
- ○ Emphasizes lasting protection
CDC: About HPV
- ● Positive
- ○ Specified risk with specific sexual activities (vaginal, oral, anal), not just “sex”
- ○ Total cancer cases (not just cervical)
CDC: Human Papillomavirus (HPV) Vaccine Safety
- ● Positive
- ○ Bulleted lists
- ○ Quantifies years and doses to demonstrate safety
- ○ Emphasizes continued monitoring
- ○ Addresses the lack of proof of causing infertility
CDC: Reasons to Get Vaccinated
- ● Positive
- ○ Bulleted lists
- ○ Quantifies efficacy and cancer risk
- ○ Prevention > screening
- ○ Quantifies years and doses to demonstrate safety
- ● Positive
- ○ Bulleted lists
- ○ Visual aid to represent statistics
CDC (Access currently uses this): HPV Vaccine VIS
- ● Positive
- ○ Q/A format
- ○ Actionable
- ○ Includes catch up vaccination
NYS DOH: HPV Vaccine
- ● Positive
- ○ Q/A format
- ○ Organization specific recs.
Cleveland Clinic: HPV Vaccine
- ● Positive
- ○ Great infographics and visuals
- ○ Describes importance of catch up vaccination
- ○ Q/A format
- ○ Quantifies efficacy
- ○ Emphasizes continued monitoring
- ○ Addresses misinformation
Mayo Clinic: HPV Vaccine
- ● Positive
- ○ Q/A format
National Cancer Institute: HPV and Cancer
- ● Positive
- ○ Q/A format
- ○ Great infographics and visuals
- ○ Quantifies cancer risk
- ○ Specified risk with specific sexual activities (vaginal, oral, anal), not just “sex”
- ○ Emphasizes lack of symptoms
- ○ Quantifies efficacy
- ○ Emphasizes continued monitoring
American Cancer Society: HPV Vaccines
- ● Positive
- ○ Q/A format
- ○ Quantifies years and doses to demonstrate safety
- ○ Addresses fertility question
- ○ Emphasizes continued monitoring
ACOG: Human Papillomavirus (HPV): Infection and Vaccination
- ● Positive
- ○ Q/A format
- ○ Specified risk with specific sexual activities (vaginal, oral, anal), not just “sex”
- ○ Emphasizes lack of symptoms
- ○ Quantifies years and doses to demonstrate safety
- ○ Emphasizes continued monitoring
ACOG: The HPV Vaccine is a Lifesaver
- ● Positive
- ○ Great visuals/infographic
- ○ Quantifies years and doses to demonstrate safety
Appendix 2: HPV Vaccine Flyer Outline
HPV
- ● Human papillomavirus
- ● Most common STI
- ● >200 strains
- ● 80% of people will get HPV - nearly all sexually active people
- ● Half of infections are high risk type
- ● Associated with genital warts and cancer
- ● No symptoms when infected, but years later can develop cancer (20-25 years later)
- ○ The body can fight the virus but not perfectly
- ■ Most infections go away, but 10-20% do not go away and cause problems
Cervical Dysplasia, Cervical and Other HPV Related Cancers
- ● Cancer of cervix, vagina, penis, anus, mouth and throat - 90% of these cancers are caused by HPV
- ■ Almost all cervical cancer
- ■ >90% anal cancer
- ■ 70% oropharyngeal cancer
- ■ 63% penile cancer
- ■ 75% vaginal cancer
- ■ 69% vulvar cancer
HPV Vaccine
- ● Gardasil 9- HPV 6, 11, 16, 18, 31, 33, 45, 52, 58 - 9 most common strains
- ● Approved in 2006, expanded in 2018 to 27-45 after talking to a health provider
- ● Usually given when 9-11
- ○ Best to get it before you have sex, but can still be very helpful after
- ○ If you are older than 15 when starting - 3 doses at 0, 1-2 months, 6 months
- ○ If you got one vaccine before, you don’t need to start over
Vaccine Safety
- ● Side Effects
- ○ Mild redness, swelling, soreness, muscle pain, fever, dizziness, nausea, headache
- ○ Passing out is uncommon
- ○ Research shows that it does not cause serious health problems like multiple sclerosis
- ○ One study of the long term effects comparing women in the older and younger groups
- ■ Injection-site AEs were pain, swelling, and erythema, which occurred in 86.1%, 23.3%, and 19.5% of women aged 16–26 years, and 82.8%, 23.3%, and 16.9% of women aged 27–45 years, respectively
- ■ Systemic AEs were headache, pyrexia, and fatigue occurring in 12.6%, 3.0%, and 2.8% of women aged 16–26 years and 13.6%, 1.7%, and 3.4% of women aged 27–45 years.
- ■ There were no vaccine-related severe AEs, no discontinuations due to a vaccine-related AE, and no deaths
Vaccine Efficacy
- ● Prevention is better than screening for precancer
- ● A meta-analysis determined that there is strong evidence of HPV vaccination successfully preventing cervical cancer
- ○ Both the high-risk HPV infection and CIN2+ are significantly declining
- ○ Treatment for these disorders can cause scarring, preterm delivery
______________________________________________________________________
Strategies
- ● Many respondents said they did not have enough information about the HPV vaccine to make a decision → increase knowledge
- ○ After healthcare professionals, those with a self-focused decision-making role identified websites (68.3%) and information pamphlets (57.6%)
Appendix 3: English HPV Vaccine Flyer
Appendix 4: Spanish HPV Vaccine Flyer
Appendix 5: HPV Vaccine Provider Training
Learning Objectives:
By the end of this training you will be able to:
- Name at least three elements of a successful HPV vaccine recommendation
- Be able to respond to at least three patient questions/concerns about the vaccine
- Understand the HPV vaccine flyer and your recommendation help to achieve the clinic goal of increasing HPV vaccination
- Integrate the HPV flyer into the clinic workflow.
Outline/Script for Holding Training
Introduction
- ● I noticed that there is a notable lack of patient centered HPV education materials that are appropriate for our patient population. Many of them are very wordy, use complex language, and do not provide actionable steps for patients.
- ● For a class project, I developed an HPV education flyer geared towards our patients here at Access GYN.
- ● The main idea is to integrate this flier into the clinic workflow. It is not intended to serve as a replacement for us educating patients, but is designed to supplement our recommendation.
- ● The goal with this initiative is to increase HPV vaccination at Access, so we achieve our clinic wide initiative of getting more patients fully vaccinated.
- ● Part of my project is to develop a training session to introduce residents and students to the flyer and discuss how to use it successfully. This is what I am piloting with you today and I would appreciate any feedback you have for me! We will talk more about strategy for how to translate your HPV knowledge into
How I Developed It
- ● I started by looking through existing patient education materials from ACOG, CDC, NIH, ACS, WHO, etc.
- ○ I assessed these for the material they contained and how they conveyed that material
- ■ I made note of pros and cons for each, and kept tally on what I was seeing and which strategies I found to be successful
What I Learned
- ● Provider recommendation is a known predictor of HPV vaccine uptake according to several studies
- ○ You recommendation to your patient is important
Reviewing the Flyer
- ● Two page, front and back flyer
- ● Meant to appeal specifically to our patients
- ○ Uninsured
- ○ 20-40s
- ○ Readability- 6th grade reading level
Using the Flyer
- ● When to give the flyer to the patient
- ○ Ideally they have it before you come in to take a history so they have time to look it over
- ○ In reality with the workflow of the clinic, it may be that you give it to them when you're in the room
Do you have any questions or concerns?
Training Activities - it can be helpful to practice and talk about previous experience, so let’s try
- ● Scenarios to role play
- ○ Introducing the vaccine
- ■ You’ve finished your history and physical and you see that the patient has the flyer already. How would you introduce the subject?
- ■ You notice your patient doesn’t have the flyer yet. What would you say when you give them the flyer?
Appendix 6: Tip Sheet
Using the HPV Vaccine Flyer for Access GYN Tip Sheet
- ● Your recommendation is important to your patient! Be sure to stress that you recommend this vaccine for them.
- ● Assess their current understanding
- ○ You don’t want to talk over their head but you also don’t want to lose their attention by saying everything they already know
- ● Personalize your recommendation
- ○ Tell them they can still benefit from it if they are already sexually active.
- ○ If a patient has had HPV and/or cervical dysplasia before, emphasize the importance of protecting against other strains.
- ● Emphasize that the benefits outweigh the risks.
- ○ Highlight the high effectiveness → >90% reduction in related cancer is significant.
- ○ Highlight that the vaccine is safe after many years of study.
- ● Decrease the barriers to vaccination
- ○ Emphasize that it’s free
- ○ Emphasize that they can get it today or at their next appointment
- ● Refer to a specific section of the flyer when answering questions to reinforce what you are saying.
- ● Encourage the patient to share the flyer with others who would benefit.
References
Ashing, K. T., Carrington, A., Ragin, C., & Roach, V. (2017). Examining HPV- and HPV vaccine-related cognitions and acceptability among US-born and immigrant Hispanics and US-born and immigrant non-Hispanic Blacks: a preliminary catchment area study. Cancer Causes & Control: CCC, 28(11), 1341–1347. https://doi.org/10.1007/s10552-017-0973-0
CDC. (2024a, July 15). About HPV. Human Papillomavirus (HPV). https://www.cdc.gov/hpv/about/index.html
CDC. (2024b, July 15). Five ways to boost vaccination rates. Human Papillomavirus (HPV). https://www.cdc.gov/hpv/hcp/vaccination-considerations/boost-rates.html
CDC. (2024c, July 15). Impact of the HPV vaccine. Human Papillomavirus (HPV). https://www.cdc.gov/hpv/vaccination-impact/index.html
CDC. (2024d, October 2). HPV educational tools and resources. Human Papillomavirus (HPV). https://www.cdc.gov/hpv/hcp/educational-resources/index.html
CDC. (2024e, December 19). Reasons to get vaccinated. Human Papillomavirus (HPV). https://www.cdc.gov/hpv/vaccines/reasons-to-get.html
CDC. (2025a, March 3). Cancers caused by HPV. Human Papillomavirus (HPV). https://www.cdc.gov/hpv/about/cancers-caused-by-hpv.html
CDC. (2025b, March 6). Human Papillomavirus (HPV). Vaccine Safety. https://www.cdc.gov/vaccine-safety/vaccines/hpv.html
CDC. (2025c, April 16). HPV vaccine VIS. Vaccines & Immunizations. https://www.cdc.gov/vaccines/hcp/current-vis/hpv.html
CDC MMWR. (2021). QuickStats: Percentage* of adults aged 18-26 years who ever received a human Papillomavirus vaccine,† by race and Hispanic origin§ and sex - national health interview survey, United States, 2019. MMWR. Morbidity and Mortality Weekly Report, 70(21), 797. https://doi.org/10.15585/mmwr.mm7021a5
Drolet, M., Bénard, É., Pérez, N., Brisson, M., & HPV Vaccination Impact Study Group. (2019). Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. Lancet, 394(10197), 497–509. https://doi.org/10.1016/S0140-6736(19)30298-3
Galvin, A. M., Garg, A., Griner, S. B., Moore, J. D., & Thompson, E. L. (2023). Health literacy correlates to HPV vaccination among US adults ages 27-45. Journal of Cancer Education: The Official Journal of the American Association for Cancer Education, 38(1), 349–356. https://doi.org/10.1007/s13187-021-02123-x
Gilkey, M. B., Calo, W. A., Moss, J. L., Shah, P. D., Marciniak, M. W., & Brewer, N. T. (2016). Provider communication and HPV vaccination: The impact of recommendation quality. Vaccine, 34(9), 1187–1192. https://doi.org/10.1016/j.vaccine.2016.01.023
Guidelines for effective writing. (n.d.). Retrieved April 28, 2025, from https://www.cms.gov/training-education/learn/find-tools-to-help-you-help-others/guidelines-for-effective-writing
HPV and cancer. (2019, March 1). https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer
HPV vaccine. (2023, August 28). Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/21613-hpv-vaccine
HPV vaccine: Who needs it, how it works. (n.d.). Mayo Clinic. Retrieved April 28, 2025, from https://www.mayoclinic.org/diseases-conditions/hpv-infection/in-depth/hpv-vaccine/art-20047292
HPV vaccines. (n.d.). Retrieved April 28, 2025, from https://www.cancer.org/cancer/risk-prevention/hpv/hpv-vaccines.html
Human Papillomavirus (HPV): Infection and Vaccination. (n.d.). Retrieved April 28, 2025, from https://www.acog.org/womens-health/faqs/hpv-vaccination
Joura, E. A., Ulied, A., Vandermeulen, C., Rua Figueroa, M., Seppä, I., Hernandez Aguado, J. J., Ahonen, A., Reich, O., Virta, M., Perino, A., Peris Tuser, M., Peters, K., Origoni, M., Raspagliesi, F., Tjalma, W. A. A., Tummers, P., Woelber, L., Nieminen, P., van Damme, P., … Wittke, F. (2021). Immunogenicity and safety of a nine-valent human papillomavirus vaccine in women 27-45 years of age compared to women 16-26 years of age: An open-label phase 3 study. Vaccine, 39(20), 2800–2809. https://doi.org/10.1016/j.vaccine.2021.01.074
Khalid, K., Lee, K. Y., Mukhtar, N. F., & Warijo, O. (2023). Recommended interventions to improve human Papillomavirus vaccination uptake among adolescents: A review of quality improvement methodologies. Vaccines, 11(8). https://doi.org/10.3390/vaccines11081390
Manhart, L. E., Burgess-Hull, A. J., Fleming, C. B., Bailey, J. A., Haggerty, K. P., & Catalano, R. F. (2011). HPV vaccination among a community sample of young adult women. Vaccine, 29(32), 5238–5244. https://doi.org/10.1016/j.vaccine.2011.05.024
McBride, K. R., & Singh, S. (2018). Predictors of adults’ knowledge and awareness of HPV, HPV-associated cancers, and the HPV vaccine: Implications for health education. Health Education & Behavior: The Official Publication of the Society for Public Health Education, 45(1), 68–76. https://doi.org/10.1177/1090198117709318
McClung, N. M., Gargano, J. W., Park, I. U., Whitney, E., Abdullah, N., Ehlers, S., Bennett, N. M., Scahill, M., Niccolai, L. M., Brackney, M., Griffin, M. R., Pemmaraju, M., Querec, T. D., Cleveland, A. A., Unger, E. R., Markowitz, L. E., & HPV-IMPACT Working Group. (2019). Estimated number of cases of high-grade cervical lesions diagnosed among women - United States, 2008 and 2016. MMWR. Morbidity and Mortality Weekly Report, 68(15), 337–343. https://doi.org/10.15585/mmwr.mm6815a1
Muthukrishnan, M., Loux, T., Shacham, E., Tiro, J. A., & Arnold, L. D. (2022). Barriers to human papillomavirus (HPV) vaccination among young adults, aged 18-35. Preventive Medicine Reports, 29(101942), 101942. https://doi.org/10.1016/j.pmedr.2022.101942
No title. (n.d.). Retrieved April 28, 2025, from https://www.health.ny.gov/diseases/communicable/human_papillomavirus/
Plain language words. (n.d.). Retrieved April 28, 2025, from https://www.ahrq.gov/health-literacy/improve/precautions/tool4e.html
Polonijo, A. N., Mahapatra, D., & Brown, B. (2022). “I thought it was just for teenagers”: Knowledge, attitudes, and beliefs about HPV vaccination among women aged 27 to 45. Women’s Health Issues: Official Publication of the Jacobs Institute of Women’s Health, 32(3), 301–308. https://doi.org/10.1016/j.whi.2022.01.007
Rincon, N. L., McDowell, K. R., Weatherspoon, D., Ritchwood, T. D., Rocke, D. J., Adjei Boakye, E., & Osazuwa-Peters, N. (2024). Racial and ethnic disparities in human papillomavirus (HPV) vaccine uptake among United States adults, aged 27-45 years. Human Vaccines & Immunotherapeutics, 20(1), 2313249. https://doi.org/10.1080/21645515.2024.2313249
Sonawane, K., Garg, A., Meissner, E. G., Damgacioglu, H., Hill, E., Nyitray, A. G., & Deshmukh, A. A. (2024). Human Papillomavirus vaccination among young adults before and during the COVID-19 pandemic. JAMA Network Open, 7(2), e2356875. https://doi.org/10.1001/jamanetworkopen.2023.56875
The HPV vaccine: Access and use in the U.S. (2024, August 5). KFF. https://www.kff.org/womens-health-policy/fact-sheet/the-hpv-vaccine-access-and-use-in-the-u-s/
The HPV Vaccine is a Lifesaver. (n.d.). Retrieved April 28, 2025, from https://www.acog.org/womens-health/infographics/the-hpv-vaccine-is-a-lifesaver
The Patient Education Materials Assessment Tool (PEMAT) and user’s guide. (n.d.). Retrieved April 28, 2025, from https://www.ahrq.gov/health-literacy/patient-education/pemat.html
Thompson, E. L., Wheldon, C. W., Rosen, B. L., Maness, S. B., Kasting, M. L., & Massey, P. M. (2020). Awareness and knowledge of HPV and HPV vaccination among adults ages 27-45 years. Vaccine, 38(15), 3143–3148. https://doi.org/10.1016/j.vaccine.2020.01.053
UpToDate. (n.d.-a). Retrieved April 28, 2025, from https://www.uptodate.com/contents/human-papillomavirus-hpv-vaccine-beyond-the-basics?search=gardasil&source=search_result&selectedTitle=3~95&usage_type=default&display_rank=2
UpToDate. (n.d.-b). Retrieved April 28, 2025, from https://www.uptodate.com/contents/human-papillomavirus-hpv-vaccine-the-basics?search=gardasil&source=search_result&selectedTitle=2~95&usage_type=default&display_rank=1
What I tell every patient about the HPV vaccine. (n.d.). Retrieved April 28, 2025, from https://www.acog.org/womens-health/experts-and-stories/the-latest/what-i-tell-every-patient-about-the-hpv-vaccine
Wheldon, C. W., Garg, A., Galvin, A. M., Moore, J. D., & Thompson, E. L. (2021). Decision support needs for shared clinical decision-making regarding HPV vaccination among adults 27-45 years of age. Patient Education and Counseling, 104(12), 3079–3085. https://doi.org/10.1016/j.pec.2021.04.016
(N.d.). Retrieved April 28, 2025, from https://www.merck.com/product/usa/pi_circulars/g/gardasil_9/gardasil_9_ppi.pdf
Post a comment